A clear guide to ranitidine: what it does, why it was recalled, dosing basics, safety concerns, and safe alternatives for acid‑related conditions.
Read MoreRanitidine: What You Need to Know
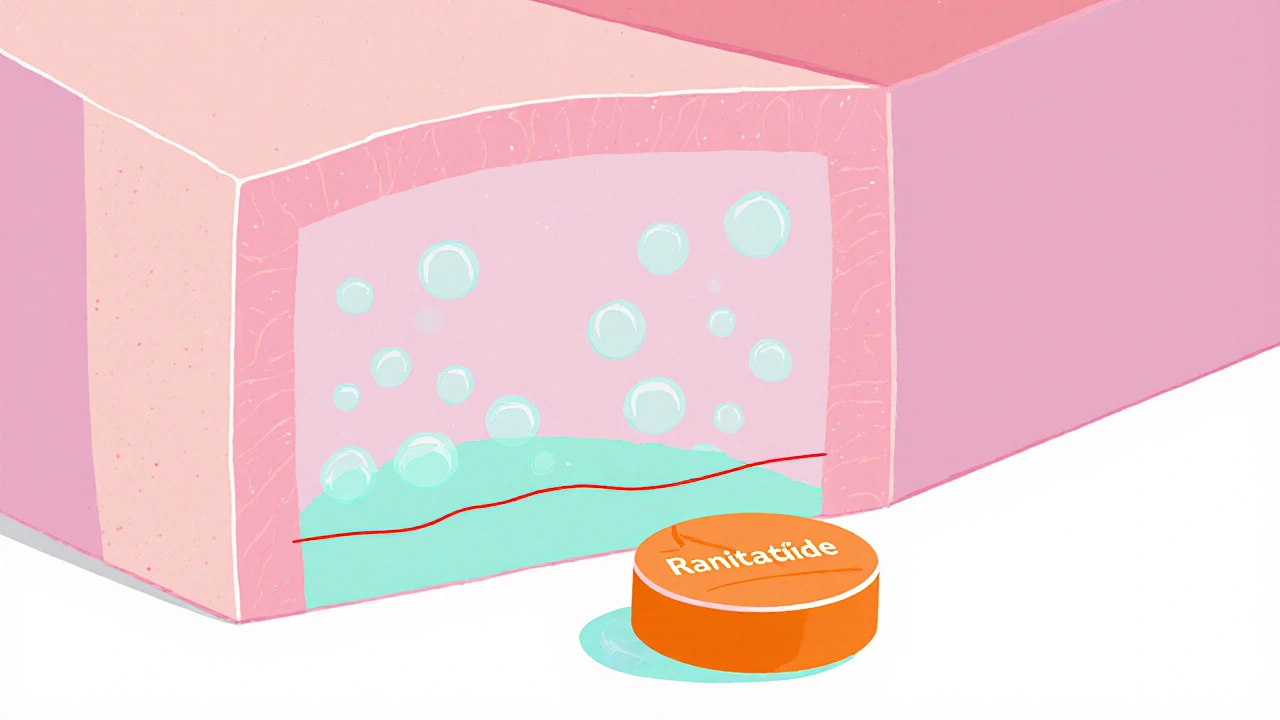
When dealing with stomach‑acid issues, Ranitidine, an H2‑receptor antagonist that lowers acid production. Also known as Zantac, it has been a go‑to option for heartburn and ulcer relief for decades.
Ranitidine belongs to the broader class of H2 blockers, drugs that block histamine H2 receptors in the stomach lining. By stopping histamine from signaling, these meds cut acid output without the stronger suppression seen in other families. Acid reflux, the backward flow of stomach acid into the esophagus often triggers the need for an H2 blocker, especially when symptoms are mild to moderate.
Common Uses and Safety Considerations
Ranitidine is typically prescribed for gastro‑esophageal reflux disease (GERD), heartburn, and treatment or prevention of gastric and duodenal ulcers. It works by reducing the volume of acid that contacts the stomach lining, which helps ulcers heal faster and eases the burning sensation of reflux. Compared with antacids, which neutralize acid already present, ranitidine tackles the problem at its source.
One key semantic link: Ranitidine reduces stomach acid → lower acid means fewer ulcer complications. Another: Acid reflux is treated with H2 blockers → ranitidine serves that role. A third: Proton pump inhibitors (PPIs) are alternatives to ranitidine → they provide stronger acid suppression for severe cases. These triples show how the drug fits into the broader acid‑control landscape.
In recent years, regulatory agencies have scrutinized ranitidine for the presence of NDMA, a probable carcinogen. Some batches were recalled, and many manufacturers halted production. This history matters because it influences current prescribing habits and patient confidence. If you’re considering ranitidine, ask your pharmacist whether the product you receive has passed the latest safety tests.
Dosage forms range from low‑dose OTC tablets (75 mg) to higher‑strength prescription tablets (150 mg, 300 mg) and liquid suspensions. The choice depends on the severity of symptoms and whether you need continuous night‑time control. Generally, adults take 150 mg twice daily or 300 mg once at bedtime; children receive weight‑based dosing under medical guidance.
Drug interactions are another practical concern. Ranitidine can affect the absorption of drugs that need an acidic environment, such as ketoconazole or iron supplements. It also may increase blood levels of certain antivirals and chemotherapy agents. Always list your current medications to your doctor to avoid unwanted effects.
People with severe liver disease, kidney impairment, or who are pregnant should use ranitidine only if the benefits outweigh the risks. The medication crosses the placenta, and while data are limited, most clinicians prefer alternatives like famotidine during pregnancy.
Side effects are usually mild: headache, dizziness, or a dry mouth. Rarely, patients report severe allergic reactions or cardiac arrhythmias. Monitoring involves checking for persistent abdominal pain, unexpected weight loss, or new gastrointestinal bleeding—signals that warrant immediate medical attention.
Below you’ll find a curated collection of articles that dive deeper into ranitidine’s alternatives, dosing nuances, safety updates, and how it compares with other acid‑reducing drugs. Whether you’re a patient looking for clear guidance or a health professional seeking the latest research, the posts ahead will give you actionable insights and up‑to‑date information.