Managing diabetes isn’t about cutting out carbs entirely-it’s about knowing exactly how much you’re eating and how it affects your blood sugar. That’s where carbohydrate counting comes in. It’s not a diet. It’s not a restriction. It’s a tool. And if you’re on insulin or trying to get your blood sugar under control, it’s one of the most powerful tools you can learn.
Why Carb Counting Works
Carbs turn into glucose. That’s it. Whether it’s bread, rice, fruit, or yogurt, your body breaks them down into sugar that enters your bloodstream. For someone without diabetes, insulin handles it smoothly. For someone with diabetes, that sugar builds up unless you match it with the right amount of insulin or other medication. Carb counting gives you control. Instead of guessing if a meal will spike your blood sugar, you calculate the grams of carbs and adjust your insulin accordingly. Studies show people who count carbs consistently see their A1C drop by 0.5% to 1.0%-a big deal when your goal is under 7%. This isn’t just for type 1 diabetes. Many people with type 2 diabetes who take insulin also benefit. Even if you’re on pills, knowing your carb intake helps you understand why your sugar goes up after certain meals.What Counts as One Carb Serving?
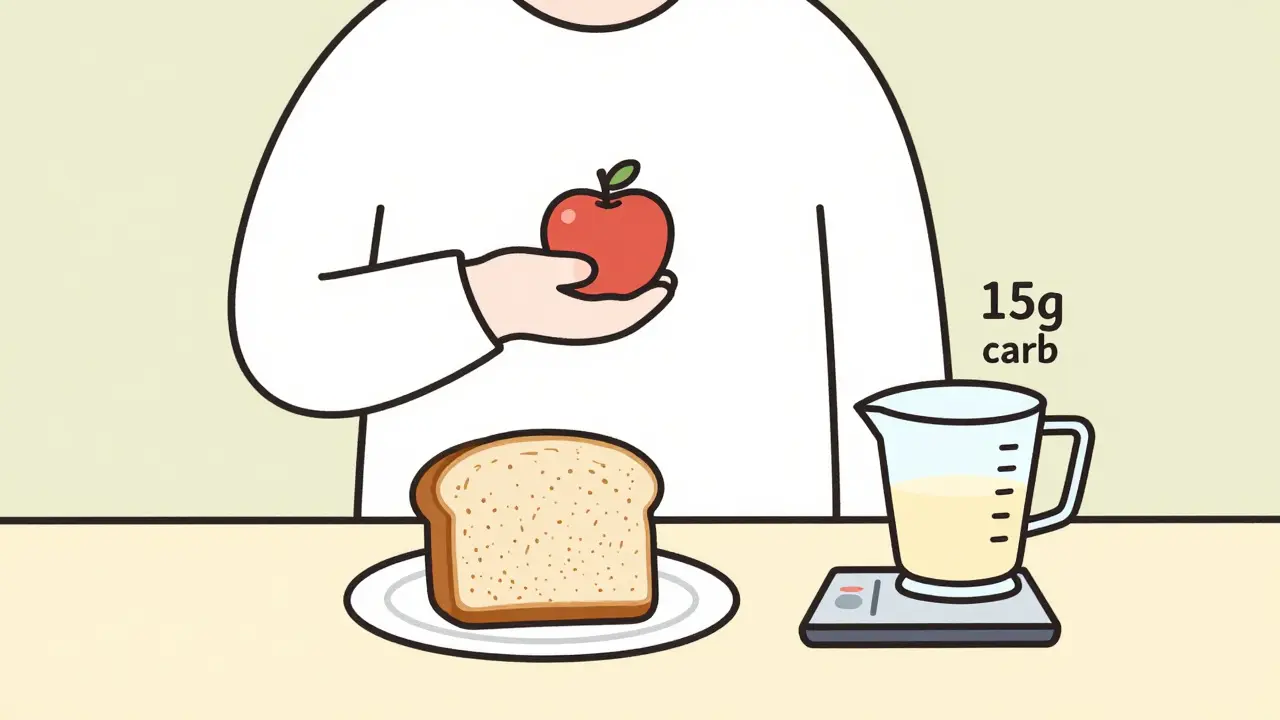
Carbs are measured in grams. The standard serving size is 15 grams. That’s the number you’ll hear from dietitians and diabetes educators. Here’s what 15 grams of carbs looks like in real life:- 1 small apple (about the size of a tennis ball)
- 1 slice of whole wheat bread
- 1/2 cup of cooked pasta or rice
- 1/2 cup of canned beans or lentils
- 1 cup of milk or plain yogurt
- 1/3 cup of cooked oatmeal
Reading Nutrition Labels Like a Pro
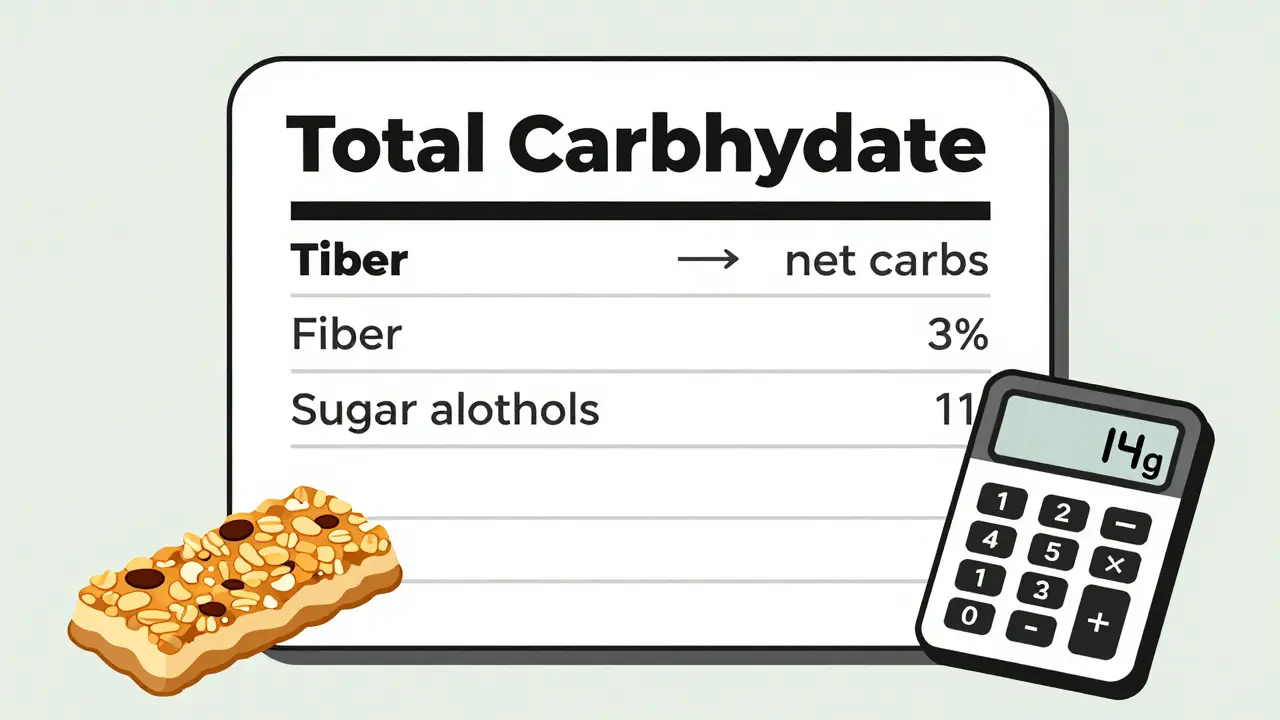
Look at the nutrition facts panel. Find “Total Carbohydrate.” That’s your number. Ignore “Sugars” and “Fiber” for now-they’re part of the total. But here’s the trick: fiber and sugar alcohols don’t affect blood sugar the same way. If a food has 5 grams or more of fiber, subtract the full amount from total carbs. Same with sugar alcohols-divide them by two and subtract that number. Example: A granola bar has 24 grams of total carbs, 6 grams of fiber, and 8 grams of sugar alcohols. 24 - 6 = 188 ÷ 2 = 4
18 - 4 = 14 grams of net carbs That’s your real carb count. This matters a lot with protein bars, keto snacks, and sugar-free products.
Your Carb-to-Insulin Ratio
If you take insulin, this is the key. Your doctor or diabetes educator will give you a ratio. It tells you how many grams of carbs one unit of insulin covers. Common ratios:- 1:10 → 1 unit of insulin for every 10 grams of carbs
- 1:15 → 1 unit for every 15 grams
- 1:20 → 1 unit for every 20 grams
What About the Plate Method or Glycemic Index?
You might have heard of the plate method-fill half your plate with non-starchy veggies, a quarter with protein, a quarter with carbs. It’s simple. But it doesn’t tell you how many grams you’re eating. That’s fine if you’re not on insulin. But if you are, you need numbers. Glycemic index (GI) tells you how fast a carb raises blood sugar. But it ignores quantity. A small serving of watermelon (low GI) might have less impact than a large serving of brown rice (medium GI). Carb counting gives you both: quantity and context.Tools You Need to Start
You don’t need fancy gear. But you do need these:- A food scale (a $15 kitchen scale works)
- Measuring cups and spoons
- A calculator (or your phone)
- A food diary or app
Common Mistakes (And How to Avoid Them)
Most beginners make the same errors:- Forgetting milk and yogurt. One cup of milk = 12 grams of carbs.
- Ignoring starchy veggies. Corn, peas, potatoes, and winter squash count as carbs.
- Assuming “sugar-free” means “no carbs.” Sugar alcohols still count.
- Not counting restaurant meals. A “small” burger bun might be 30 grams. A side of fries? 40+ grams.
- Not adjusting for insulin sensitivity. Your body needs more insulin in the morning than at night.
Real Results: What People Actually Experience
On Reddit’s r/diabetes, one user wrote: “My post-meal spikes went from 250+ to 160-180 in two weeks. I finally felt in control.” Another said: “I used to avoid pizza. Now I count the carbs, take my insulin, and enjoy it. No guilt.” A study from the Journal of Diabetes Science and Technology found that after 30 days of consistent carb counting, people got 85% accurate at estimating carbs. That’s the goal. One patient reduced their A1C from 8.9% to 6.2% in 18 months-not by cutting carbs, but by matching them with insulin.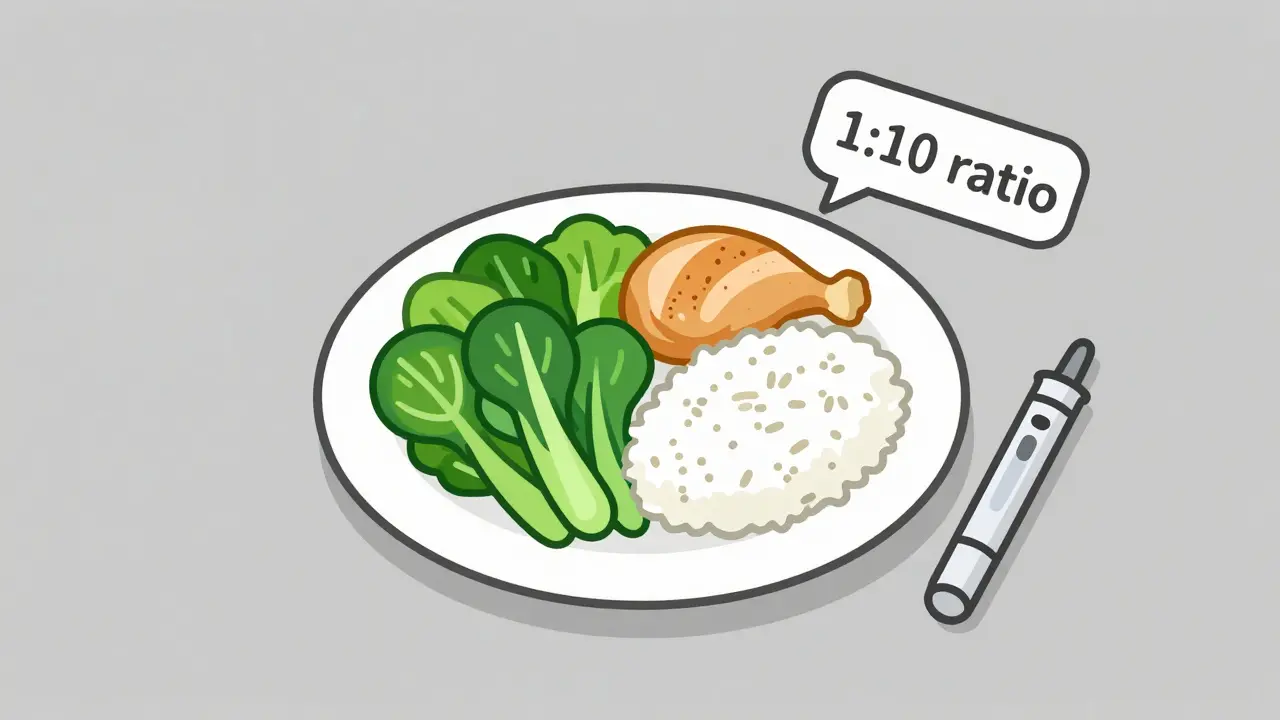
When You’re Eating Out
Restaurants are tricky. Portion sizes are huge. Labels are often wrong. Here’s how to handle it:- Check chain restaurant websites. McDonald’s, Starbucks, Chipotle all list nutrition info.
- Ask for sauces and dressings on the side.
- Split an entrée or take half home.
- Use your app to scan the food if it has a barcode.
- When in doubt, estimate low and check your blood sugar 2 hours later.




15 Comments
Carb counting changed my life. I used to dread meals. Now I plan them. No more spikes. No more guilt. Just control.
It’s not perfect but it’s mine.
i always forget the fiber thing and then wonder why my bg is low after eating those ‘keto’ bars lol
thanks for the reminder
So you’re telling me I don’t have to give up pizza?
Wow. I think I just found my new favorite hobby.
As someone who grew up eating rice with every meal, this guide felt like a lifeline.
My grandma still thinks diabetes means no rice. I showed her the 1/2 cup serving.
She cried. Then she made me a bowl.
With extra ghee. But I counted it. And took my insulin.
Freedom isn’t about denying your culture. It’s about owning it.
💯 This is the best guide I’ve ever read.
Finally someone who gets it.
And yes I used emojis because I’m proud of this.
My A1C dropped from 8.1 to 6.9 in 4 months thanks to this.
Thank you for writing this.
Carbs aren’t the enemy. Fear is.
We’ve been taught to hate food because of numbers.
But the truth? The body doesn’t hate sugar.
It hates being ignored.
When you count carbs, you’re not punishing yourself.
You’re listening.
You’re asking: ‘What do you need?’
And then you answer.
That’s not discipline.
That’s love.
I’ve been doing this for 3 years. Here’s the secret nobody tells you: you don’t need to be perfect.
Some days you’ll miscount. Some days you’ll eat a whole bag of chips and just check your sugar.
That’s okay.
What matters is you showed up.
That’s more than most people with diabetes do.
Keep going. You’re doing better than you think.
As a certified diabetes educator in Mumbai, I have witnessed the transformative power of carbohydrate counting in patients who were previously resigned to poor glycemic control.
Many patients, particularly those from lower socioeconomic backgrounds, initially perceive this method as overly complex or Western-centric.
However, when taught with culturally relevant examples - such as measuring a chapati as one carb serving, or recognizing that a single banana equals two servings - they rapidly gain confidence.
Consistency, not perfection, is the cornerstone.
Moreover, the integration of smartphone applications with localized food databases has dramatically improved adherence.
Patients report not only improved HbA1c levels but also renewed psychological autonomy.
This guide is exemplary in its clarity and practicality.
I will be distributing this to all my trainees and patients.
Thank you for this invaluable contribution to diabetes self-management education.
why do i need to count carbs when i could just take more insulin?
lazy.
so you’re saying i can eat cake if i count the carbs?
oh hell no. i’m not doing math before dessert.
you’re all just sugar addicts pretending to be scientists.
i read this at 3am after a 280 spike.
it didn’t fix my blood sugar.
but it made me feel less alone.
thank you.
THIS IS A BIG PHARMA SCAM.
They want you to think you need to count carbs so you’ll keep buying insulin and apps.
Real healing is in fasting. In keto. In rejecting modern medicine.
They don’t want you to know the truth.
They profit from your confusion.
Wake up.
They’re lying to you.
how do you know if your insulin ratio is right?
do you just guess until your sugar’s not crazy?
carbs are a liberal plot to make diabetics dependent on insulin.
real Americans eat meat and butter.
if you’re counting carbs, you’re already lost.
get off the sugar train before it’s too late.
the government doesn’t want you healthy.
they want you medicated.
i think the FDA is hiding the truth about fiber and sugar alcohols.
why do they let companies lie on labels?
and what if the app databases are corrupted?
what if my phone is spying on my blood sugar?
i’m not trusting anything anymore.
maybe i should just eat nothing.
or maybe i should move to the woods.
and stop using phones.
and stop trusting doctors.
and stop trusting this post.
...but i still counted my carbs today.
just in case.