How Do You Know If a Child's Anxiety Is Serious—and What Are the Signs?
Kids worry—about monsters, about their first swimming lesson, sometimes about whether you’ll be late picking them up. But when does anxiety cross the line and actually need medical help or medication like hydroxyzine for children? Most parents wrestle with this at some point, especially when the world just feels stressful. The difference between everyday nerves and an anxiety disorder usually comes down to intensity, frequency, and disruption. If your child’s worries stop them from going to school, sleeping, playing, making friends, or trying things they used to love, you might be dealing with something more than just a phase. We’re not talking about one meltdown at a birthday party; think patterns that last for weeks, even months, and lead to real changes in their behaviour or mood.
Doctors call these ‘functional impairments’ — the fancy term for real-life obstacles. The official criteria (from the DSM-5, which guides mental health diagnoses) say you should watch for symptoms like recurring panic, constant ‘what if’ worries, headaches or stomachaches with no clear cause, and a child who avoids things they used to face with ease. Kids might start avoiding the dinner table, refusing to go to school, or become so clingy you can’t leave the room. Sometimes, the physical signs stand out first: headaches, belly pain, sleeping badly, or just seeming ‘on edge’ all the time. It’s not just shyness—true anxiety can paralyse, not just nudge.
The truth? Anxiety disorders affect up to 10-20% of children at some point, and the numbers have gone up since the pandemic. This isn’t rare. So if you suspect your child’s anxiety is causing serious distress, it’s not an isolated problem—and you’re not a ‘bad parent’ for running into this. Assessment isn’t a guessing game: clinicians look for a combination of severe worry, avoidance, physical symptoms, and how much it actually gets in the way of your child living like a kid. They’ll tease apart if the anxiety is specific (like only before a test or meeting new people), or happens all the time, everywhere. If your child is hitting these marks, that’s when it’s worth talking to a specialist. Sometimes paediatricians run bloodwork first, just to rule out physical things (like thyroid issues or anaemia) that could cause similar symptoms.
Not every anxious child will need medication. It’s usually saved for when therapy isn’t enough, or the symptoms are so big—panic attacks, crushing separation anxiety, or daily meltdowns—that waiting for therapy to kick in might do more harm. Hydroxyzine isn’t always the first choice—more on that in a bit—but it is prescribed for kids who are really struggling to function in daily life, and when the anxiety feels overwhelming. Clinicians weigh risk and benefit carefully, especially for young kids. There’s never a ‘just in case’ prescription when it comes to psychiatric meds for children.
It’s so important to remember that anxiety has many faces. Some children act out, others withdraw. Boys are more likely to show anger or defiance, while girls might become quieter and people pleasing. No wonder parents feel confused—it doesn’t look the same in every household. There’s no shame in getting a clinician’s take, and sometimes just naming what’s going on makes all the difference.
Anxiety is also sticky: untreated, it tends to hang around and sometimes grow up as depression, school refusal, or even substance use in late teens. Spotting it, getting help, and knowing the signs is genuinely one of the most important things you can do as a parent. Trust your instincts—they’re so often right.

Clinical Criteria for Using Hydroxyzine: Who Gets It and Why?
So, what’s the real story behind using hydroxyzine for children? Hydroxyzine is an antihistamine (more commonly found treating allergies), but in the UK and elsewhere, it’s sometimes used off-label to tackle short-term anxiety in kids. This isn’t usually the ‘go to’ anxiety med—those are usually SSRIs like sertraline—but there are really specific moments when hydroxyzine makes sense. If you’re curious about whether it’s safe and when it should be considered, check the detailed breakdown on hydroxyzine for child anxiety.
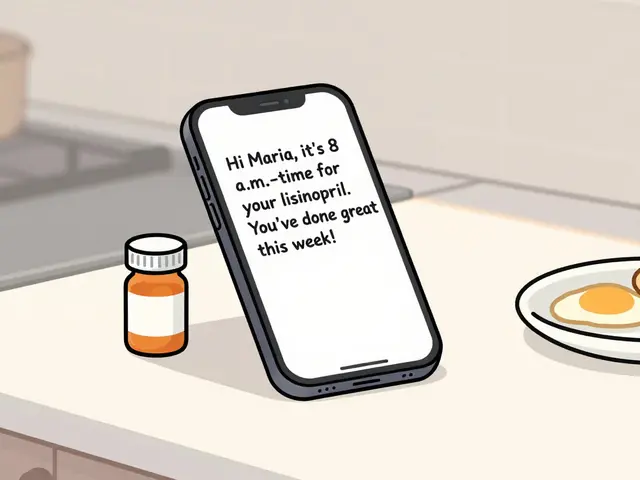
Doctors typically reach for hydroxyzine in a handful of situations. Maybe a child needs something fast-acting before a medical procedure or major event (MRI scan, first day at a new school, dental work—moments that are too big for basic coping skills to handle). Or, it’s prescribed for ongoing, severe anxiety when therapies aren’t working quickly enough and the child is really struggling to function. It kicks in within 30-60 minutes and doesn’t have the long-term side effects that can come with antidepressants. But it’s not a cure and it doesn’t solve ongoing anxiety—think of it as a temporary life raft, not a boat you live on. Most guidelines put clear limits on how long it should be used, often days to a few weeks, never months on end.
Hydroxyzine’s biggest plus? Low risk of dependence and very few interactions with other medicines kids might take. Also, unlike benzodiazepines (which most GPs wouldn’t dream of prescribing to children, for good reason), hydroxyzine is much less likely to cause sedation, memory issues, or dependency. For short-term, acute anxiety—think panic before an operation or a really tough family event—it’s a practical tool. The NHS, for instance, approves it only for limited scenarios, and only after ruling out other non-drug options. The dose for children is always carefully calculated by weight—not an at-home guess—and parents are given strict instructions not to use adult doses or repeat too often. You definitely want a paediatrician or child psychiatrist making these calls, not your own best guess off the internet.
There are, of course, important clinical rules. Doctors will ask about heart conditions, history of seizures, and all other medicines the child is on, because there’s a very rare but serious risk of heart rhythm issues. Side effects most children actually experience? Sleepiness (a blessing if the anxiety is stopping them sleep), a dry mouth, and the odd mild headache. Most don’t get anything more serious than that, but everyone reacts differently. If a child gets unusually groggy, dizzy, or develops a rash, you stop and call the doctor. Hydroxyzine is never a substitute for therapy or strong parent support—but for the small chunk of children who need immediate relief, it can be a bridge to more lasting solutions.
Doctors in the UK still consider it a ‘last resort’ for ongoing anxiety. The NICE guidelines, which shape best practice, favour therapy (CBT, mindfulness training, family work) first, followed by SSRIs if things don’t improve. For severe cases—panic attacks, obsessive rumination, avoidance so bad a child can’t go to school—a brief course of hydroxyzine is sometimes used while waiting for therapy to start. And even then, only after parents have tried solid coping strategies at home and in school. It’s not for light touch worry—it’s for anxiety that knocks the wind out of the family. Always go for real medical advice, not just parent chat forums, because each child’s risk factors are different.
So why do some kids respond well? Hydroxyzine blocks certain brain chemicals linked to anxiety and helps calm the nervous system almost immediately, which can be a total lifesaver in a full-blown panic spiral. But the results don’t last for weeks. It’s the safety net when your child is stuck on the high wire and can’t get down, not the training wheels they use forever. It fills a gap, but never stands alone. The research is still limited, but short studies (like one published in European Child & Adolescent Psychiatry in 2022) show that for acute moments, it reduces symptoms as well as low-dose benzodiazepines—without the addiction risks. Most paediatricians prefer CBT or mild SSRIs, but they’ll consider hydroxyzine if the need is urgent and the usual strategies just aren’t keeping a child safe or able to function.

Coping Strategies That Work—What Parents and Kids Can Do Beyond Pills
Medication doesn’t solve everything—and honestly, for the majority of anxious kids, it shouldn’t be the main event. Most young children, especially under 12, do better with the right coping skills, routines, and support systems around them. So what actually works, day-to-day? Let’s run through the evidence-backed techniques and some practical hacks you might not have tried.
- Routine and Predictability: Children thrive on predictability, especially those with anxiety. A simple, visual routine (think a whiteboard or fridge chart) helps anxious brains relax, because surprises drop by the wayside. Even in our family, Maeve finds that a calming bedtime routine with the same four steps (bath, pyjamas, books, lullaby) shaved an entire hour off our daughter’s pre-sleep anxiety. Routines signal safety—and that’s half the battle.
- Exposure—Not Avoidance: There’s a concept in therapy called ‘exposure with support’. It means you slowly guide children toward things that scare them, not away. If your child’s anxious about dogs, start with photos, then a fuzzy toy, then peek at live dogs from a safe distance. The secret? Do it in tiny steps, and celebrate progress, not perfection. Avoiding triggers always backfires—anxiety grows the more you run.
- Mindful Breathing and Grounding Exercises: Simple breathing tricks help a child ‘reset’ their body and mind. One UK school tested balloon breathing (inhale for 4, hold for 4, blow out slowly as if inflating a balloon) and found it slashed panic attacks by 60% over three months. There’s also the classic 5-4-3-2-1 game: spot five things you can see, four you can touch, three you can hear, and so on. It’s all about pulling your child back into the here-and-now when anxiety tries to yank them away.
- CBT (Cognitive Behavioural Therapy): CBT is the gold standard for paediatric anxiety. It’s not fluffy chat; it’s specific skills like ‘worry ladders’ and ‘detective thinking’. In one study from Bristol Children’s Hospital, more than 65% of anxious kids saw their symptoms drop by half after eight weeks of guided CBT—far better odds than most meds, with zero side effects. If you can access an online CBT course or a local therapist, go for it.
- Parent Training: Here’s the part nobody talks about—parents have the power to help or hinder. Training programs that teach parents to manage their own anxiety, avoid harsh discipline, and model calm responses are as effective as direct therapy for many kids. Try not to ‘over-reassure’; instead, acknowledge the worry and encourage action. “I see you’re worried about school, but I know you can do hard things. Let’s work on one step together.”
- Physical Activity: Movement releases brain chemicals that melt anxiety away. Even something as simple as a daily 20-minute walk proved to reduce anxious symptoms by a third in a University of Exeter trial. Bonus: No cost, and you get fresh air in the process.
- Sleep Hygiene: Good sleep wipes out a surprising chunk of anxiety in kids. That means a screen-free half-hour before bed, blackout curtains, and if possible, the same bedtime every night (even on weekends). Our own household is militant about blue-light blocking glasses after 7pm—it really works.
- Diet and Caffeine: Watch for sneaky sources of stimulant caffeine—colas, iced tea, unfiltered herbal remedies. Even a little bit ramps up anxiety in sensitive children. Keep meals regular, balanced, and skip sugary breakfasts if possible—they’re linked to mid-morning mood crashes.
- Creative Expression: Drawing, journaling, even acting out worries with puppets gives children an outlet that words often can’t. Art-based programs in Bristol schools have reduced anxiety rates by 22% in the last two years—a huge win for kids who struggle to talk about their feelings.
- Social Support: Isolate an anxious child, and their worries double. Safe playdates, trusted relatives checking in, and small group clubs give anxious kids a low-pressure chance to connect. If school feels overwhelming, just one understanding adult at drop-off can make the difference between panic and peace.
One unexpected tip? Let children see YOU use coping skills. When our family has a rough day, I’ll literally say, “My worries got big, so I took three deep breaths and petted the cat.” Kids learn best by copying what they see. And if you try a strategy and it flops, that’s normal—don’t toss it, tweak it. Maybe that grounding technique works better before school than after dinner; maybe what calms your youngest winds up your oldest. Adapt until it clicks for your unique child.
Finally, get school involved as soon as the anxiety interferes with attendance, grades, or friendships. Teachers are trained to spot early warning signs, and most UK schools now offer pastoral support or school-based counselling. Don’t be shy—your child’s anxiety is never an inconvenience to their educators. And if your GP shrugs you off, bring in written records, school reports, and a log of symptoms. The squeaky wheel gets the referrals, plain and simple.
Hydroxyzine is a useful tool for acute, overwhelming anxiety, but it’s not a lifestyle choice for most families. Every child deserves the chance to learn coping skills, build confidence, and tackle the world with support, not sedation. Be open to the whole toolkit—and remember, there’s always hope, even when anxiety feels like it’s winning.



19 Comments
Pharmaceutical corporations have long capitalized on the anxiety epidemic, steering parents toward quick‑fix medications while minimizing the need for comprehensive behavioral interventions. The regulatory frameworks often lack the transparency needed for caregivers to make fully informed decisions. Moreover, the off‑label use of antihistamines such as hydroxyzine raises concerns about long‑term safety data in pediatric populations. Parents should scrutinize the underlying motivations behind prescribing trends rather than accepting them at face value. A critical examination of the incentives at play is essential for protecting children’s mental health.
Honestly, the whole "just give the kid a pill" mentality reeks of lazy parenting and lazy medicine. Simple routines and exposure are far more effective than a fleeting antihistamine cruise.
Our nation’s children deserve better than a Western pharmaceutical quick‑fix. It is downright irresponsible to import foreign drug policies without rigorous local scrutiny; the drama of panic attacks is not a ticket for foreign pills.
Data shows hydroxyzine has a low dependency risk but the side‑effects like drowsiness can cripple school performance.
In a multicultural context, it is vital to respect diverse coping traditions while integrating evidence‑based practices; families benefit when clinicians honor cultural narratives alongside therapeutic techniques.
When a child wakes up trembling with a racing heart and a roaring mind, the first step is to recognize the physiological loop that fuels the fear
Instead of rushing to a prescription, we can gently guide them through grounding exercises that anchor them in the present moment
Simple breathing techniques, like the 4‑7‑8 method, can recalibrate the nervous system within minutes and reduce cortisol spikes
Consistent bedtime rituals signal safety to the brain, allowing the parasympathetic system to dominate over the fight‑or‑flight response
Physical activity, even a short walk, releases endorphins that naturally counteract anxiety signals
Therapeutic exposure, done gradually, teaches the child that feared stimuli are tolerable and not catastrophic
When these behavioral strategies are employed daily, the reliance on medication diminishes dramatically
Parents who model calm behavior provide a mirror for their children to emulate, reinforcing the coping toolkit
Involving schools in creating predictable schedules and safe spaces further consolidates these gains
While hydroxyzine offers short‑term relief, it should be viewed as a bridge, not a destination, and only after non‑pharmacologic methods have been maximized
Each child’s response is unique, so continuous observation and adjustment of strategies are paramount
Professional guidance from child psychologists can tailor interventions to individual neurodevelopmental profiles
Collaborative care, integrating pediatricians, therapists, and families, yields the most robust outcomes
Ultimately, fostering resilience equips children to navigate future stressors with confidence and reduced dependence on medication.
Picture this: a kid swamped by a cascade of worries, and the doctor hands over a sedative that feels like a magic wand. Spoiler: the wand breaks after a week, leaving the kid more jittery than before. Real change comes from reshaping habits, not from a color‑coded tablet that promises instant calm but delivers a foggy haze.
From a mentorship perspective, it is crucial to frame hydroxyzine as a temporary adjunct rather than a primary solution. The pharmacologic effect peaks within an hour, providing a window for the child to engage in exposure tasks without overwhelming panic. During that window, clinicians should collaborate with families to practice coping skills, ensuring the medication serves as a scaffold. Additionally, monitoring cardiac rhythm is indispensable given the rare but serious arrhythmia risk. Parents must maintain a symptom diary, noting any excessive sedation, dizziness, or rash, and communicate promptly with the prescribing physician. By integrating medication with structured behavioral interventions, we preserve the child’s agency and prevent dependence on pharmaco‑therapy. This balanced approach respects both the urgency of acute anxiety relief and the long‑term goal of resilience building.
Think of anxiety as a storm that can be weather‑proofed with the right shelter. Consistent routines act as the roof, while mindful breathing is the sturdy window that lets fresh air in. When children learn to label their feelings, the storm loses its mystery and power. Encouraging creative outlets like drawing turns inner turbulence into expressive art, diffusing tension. The key is to weave these practices into daily life so they become second nature, not a forced chore.
Oh, the drama of a parent whining about a single pill while the kid’s anxiety builds like a volcano! Let’s cut the melodrama-real help comes from consistent boundaries, not from begging the doctor for a legal high.
Honestly, stepping into the conversation without a clue is like painting a masterpiece with a broom. We need evidence, not just loud opinions.
While many celebrate hydroxyzine as a miracle, I contend that the data is inconclusive and the enthusiasm is largely anecdotal. A rigorous double‑blind trial is necessary before endorsing widespread pediatric use.
Supporting kids through anxiety feels like coaching a team through a tough season; we celebrate small victories, adjust strategies, and keep the morale high.
the article feels kinda solid :) but i think we should also look at diet and sleep patterns
The philosophical angle is clear: reliance on medication risks reducing personal agency, yet the empirical evidence suggests short‑term benefits when used correctly. Balance is essential.
When considering any pharmaceutical intervention for a child, there are several layers of responsibility that must be meticulously adhered to. First, a thorough differential diagnosis is required to rule out medical conditions that can mimic anxiety, such as hyperthyroidism or anemia. Once a psychiatric diagnosis is confirmed, evidence‑based non‑pharmacologic treatments should be the foundation of care. Cognitive‑behavioral therapy, exposure exercises, and family psychoeducation have robust data supporting their efficacy in pediatric anxiety disorders. If, after a reasonable trial of these interventions, the child's functional impairment remains severe-characterized by persistent panic attacks, school refusal, or debilitating somatic complaints-then clinicians may consider an adjunctive pharmacologic agent. Hydroxyzine, with its rapid onset and low dependence potential, can serve as a short‑acting bridge while waiting for therapeutic effects of CBT to manifest. However, strict dosing based on weight, careful monitoring for sedation, and a definitive termination plan are non‑negotiable. The prescription should be accompanied by a written plan outlining the duration of use, expected outcomes, and criteria for discontinuation. In practice, this approach ensures that medication complements, rather than supplants, the core therapeutic work aimed at fostering long‑term resilience in children.
Implementing consistent bedtime routines can dramatically reduce nighttime anxiety in children.
I appreciate the thorough overview and would add that maintaining a symptom journal can help clinicians fine‑tune treatment plans over time.
While the article is comprehensive, it fails to cite the latest meta‑analysis from 2023 that delineates the comparative efficacy of hydroxyzine versus low‑dose SSRIs in pediatric populations; such an omission undermines the academic rigor expected in a scholarly discourse.