When you pick up a generic pill, you expect it to work just like the brand-name version. But behind that simple expectation is a complex, high-stakes manufacturing process where tiny errors can have big consequences. Between 2019 and 2023, generic drugs had 3.2 times more quality defects than their branded counterparts, according to FDA inspection data. These aren’t random mistakes-they’re systemic failures tied to outdated equipment, cost-cutting pressures, and insufficient oversight.
What Exactly Are Generic Drug Manufacturing Defects?
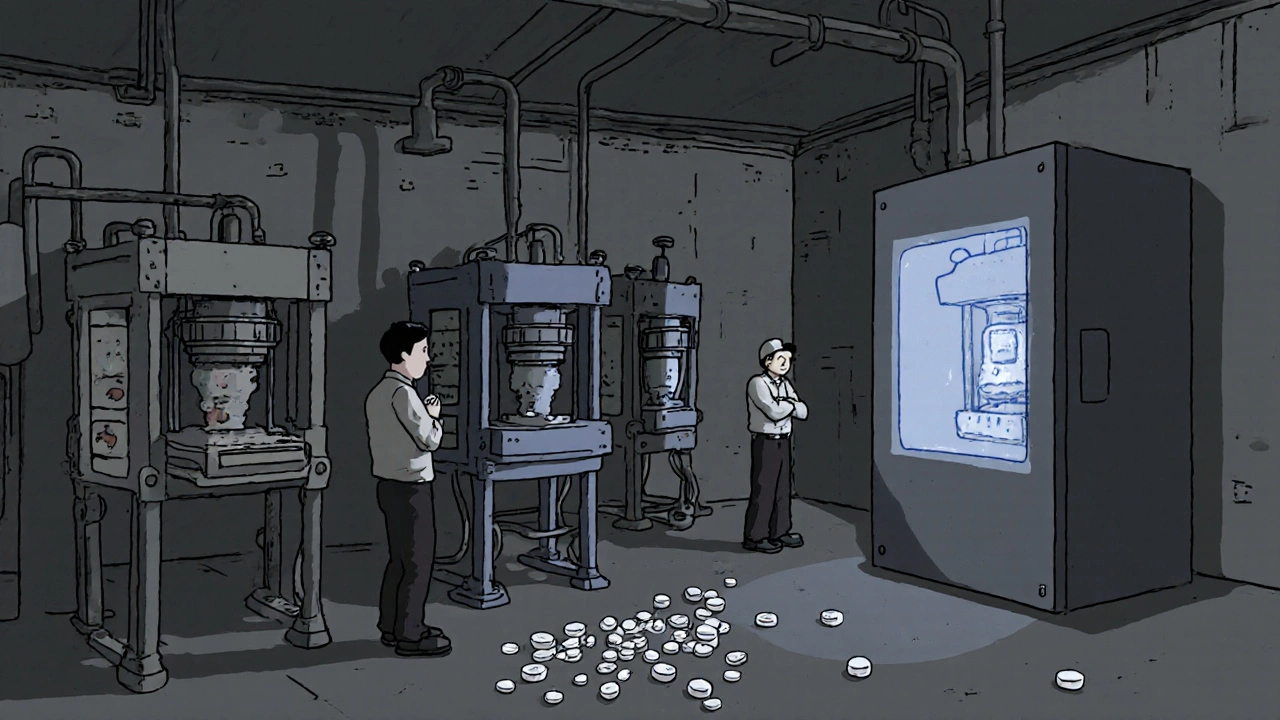
Quality defects in generic drugs fall into clear categories, each with specific causes and risks. The most common are physical flaws in tablets and capsules: capping, lamination, sticking, and mottling. Capping happens when the top of a tablet splits off horizontally. This occurs when compression force exceeds 15 kN and moisture levels in the formulation drop below 2%, especially in hydrophobic drugs. Lamination is when layers peel apart-often caused by turret speeds over 40 rotations per minute and poor pre-compression settings. Sticking occurs when the drug material clings to the punch head, increasing ejection forces by 300-500 N when active ingredients melt below 120°C and moisture exceeds 4%. Mottling, or uneven coloring, doesn’t affect potency but erodes patient trust and can signal deeper batch inconsistencies.Then there are invisible but dangerous defects: weight variation and contamination. The U.S. Pharmacopeia (USP <905>) allows no more than 5% deviation in tablet weight. But when granule flow rates fall below 0.5 g/s, 12.7% of batches fail this standard. In sterile injectables, particulate contamination is the top issue-tiny particles that shouldn’t be there can trigger immune reactions or block blood vessels. The FDA classifies these as critical defects when they affect dose accuracy, major when they damage confidence, and minor when they’re cosmetic and explainable.
Why Do These Problems Happen So Often in Generics?
The root cause isn’t incompetence-it’s economics. Generic manufacturers compete on price, not quality. While branded drugmakers spend 15-18% of production costs on quality assurance, generics average just 8-10%. That gap shows up in inspection failure rates: 57% of generic facilities failed FDA checks between 2019 and 2023, compared to 28% for branded sites. Aging equipment is another problem. Many generic plants still use tablet presses from the 1980s, with punch tolerances drifting beyond the ±0.05 mm standard. Real-time force monitoring, required to keep compression within ±10% of target, is often missing.Shared production lines make cross-contamination worse. One facility might produce an antibiotic one day and a blood pressure pill the next, with inadequate cleaning between runs. And because generics are low-margin products, companies delay equipment upgrades. The Generic Pharmaceutical Association estimates it would take $28.7 billion to modernize all U.S. generic manufacturing facilities. But annual investment is only $1.2 billion.
Which Generic Drugs Are Most at Risk?
Not all generics are created equal. Complex formulations are far more vulnerable. Inhalers have a defect rate of 18.2%, modified-release tablets 14.7%, and sterile injectables 8.7%. These require precise control over particle size, release timing, and sterility-things that are hard to replicate on cheap equipment. Even simple immediate-release tablets, with a 9.3% defect rate, aren’t safe. A 2023 Reddit thread from pharmacists described batches of metformin ER that crumbled during dispensing. Another reported patients switching between levothyroxine generics and experiencing fatigue, heart palpitations, or weight changes-signs of inconsistent absorption.Why? Because bioequivalence doesn’t guarantee therapeutic equivalence. A 2021 JAMA Internal Medicine study found 7.3% of generic drug applications failed bioequivalence testing-not because the formula was wrong, but because manufacturing inconsistencies altered how the drug dissolved in the body. The European Medicines Agency reported in 2023 that 31% of generic applications needed multiple review cycles due to quality concerns, compared to 14% for branded drugs.
What’s Being Done to Fix This?
Some manufacturers are stepping up. The FDA’s Emerging Technology Program has helped 47 generic companies switch to continuous manufacturing-a process that reduces defect rates by 65% compared to traditional batch methods. AI-powered visual inspection systems now detect defects as small as 0.1 mm at 600 tablets per minute, cutting human error from 30% to under 2%. In-line weight monitoring rejects tablets outside ±5% of target weight in real time, even at speeds of 1,200 tablets per minute.Training is also improving. Staff now get 40+ hours of GMP-specific instruction annually, with requalification tests showing 85%+ proficiency. The FDA’s Quality by Design (QbD) guidance, updated in 2022, requires manufacturers to define a “design space” for critical quality attributes-essentially mapping out the safe operating window for each step. But adoption is uneven. Only a fraction of small manufacturers have the resources to implement these systems.

How Patients and Providers Are Affected
The human impact is real. A 2023 survey of 1,247 U.S. pharmacists found 68% had seen quality issues with generics in the past year. Forty-two percent reported patients complaining about cracked, discolored, or crumbling tablets. Twenty-nine percent noted patients saying the generic “just didn’t work like before.” Hospital formulary committees recorded that 17.3% of generic substitution requests in 2023 were rejected due to quality concerns, with nearly 10% leading to permanent brand retention.The FDA’s MedWatch system received 1,842 adverse event reports in 2023 specifically citing generic drug quality-327 of them involving visible defects. These aren’t just complaints. They’re warnings. When a patient switches from one generic to another and has a bad reaction, it’s often not about the drug itself-it’s about how it was made.
What’s Next for Generic Drug Quality?
The future hinges on modernization. The 2024 Drug Supply Chain Security Act now requires enhanced tracking for high-risk generics, reducing counterfeit-related issues by 22% in early trials. AI-driven quality control pilots at Sandoz and Dr. Reddy’s are achieving 92% defect detection accuracy-far better than traditional methods. The FDA’s 2024-2027 plan aims to cut quality-related shortages by 30% through incentives for advanced manufacturing.But the road is steep. Without major investment, McKinsey & Company predicts 15-20% of generic manufacturers could exit the market in five years. The ones that survive will be those that treat quality not as a cost center, but as the foundation of trust. For patients, this means staying alert: if a generic pill looks different, tastes different, or seems to work differently, report it. Your pharmacist can help. And if your doctor recommends switching, ask: Is this the same manufacturer as before?
Generics saved the U.S. healthcare system hundreds of billions. But if we keep treating them like commodities instead of life-saving medicines, we risk losing more than money-we risk losing safety.
What are the most common physical defects in generic tablets?
The most common physical defects are capping (tablet top splitting off), lamination (layers peeling apart), sticking (drug material clinging to the punch), and mottling (uneven coloring). These are often caused by improper compression force, moisture levels, or outdated equipment. Capping happens when pressure exceeds 15 kN and moisture is below 2%. Lamination occurs at turret speeds over 40 RPM with poor pre-compression.
Why are generic drugs more prone to defects than brand-name drugs?
Generic manufacturers face intense price pressure and typically spend only 8-10% of production costs on quality assurance, compared to 15-18% for branded companies. Many use aging equipment, share production lines between drugs, and delay upgrades. This leads to higher inspection failure rates-57% for generics versus 28% for branded drugs between 2019 and 2023.
Can a generic drug still be safe if it looks different?
Appearance changes like color, shape, or markings don’t always mean the drug is unsafe-but they can signal manufacturing inconsistencies. If a tablet crumbles, chips, or has uneven coloring, it may indicate poor formulation control or moisture exposure. Patients should report these issues to their pharmacist. The FDA’s MedWatch system accepts reports of visible defects, and these help trigger investigations.
How can I tell if my generic medication has a quality issue?
Watch for changes in how the pill looks (cracking, discoloration, crumbling), feels (unusual texture), or works (new side effects, reduced effectiveness). If you notice these after switching to a new generic batch, talk to your pharmacist. They can check the manufacturer and lot number. You can also report issues directly to the FDA’s MedWatch system.
Are newer manufacturing technologies helping reduce defects?
Yes. Continuous manufacturing, AI-powered visual inspection, and real-time weight monitoring are cutting defect rates significantly. Companies using these technologies report up to 65% fewer defects than those using traditional batch methods. AI systems now detect flaws as small as 0.1 mm with 92% accuracy, compared to 78% for manual checks. But adoption is slow-only 47 generic manufacturers have joined the FDA’s Emerging Technology Program so far.
For healthcare providers, the key is vigilance. Don’t assume all generics are interchangeable. Track which manufacturer your patients are using. If a patient reports a change in response, investigate the batch. For patients, know your medication. Ask questions. Report concerns. Quality isn’t optional-it’s the foundation of every pill you take.




12 Comments
Generic drug manufacturing defects are a classic case of systemic cost optimization overriding pharmacological integrity. The physical flaws-capping, lamination, sticking-are direct artifacts of suboptimal process parameters, often exacerbated by outdated equipment. But the deeper issue lies in the lack of statistical process control. When granule flow rates dip below 0.5 g/s, you're not just risking weight variation-you're compromising dissolution kinetics. And bioequivalence studies? They're based on population averages, not individual pharmacokinetic variance. A 7.3% failure rate in BE testing means nearly 1 in 13 generics may not deliver consistent therapeutic exposure. That’s not a statistical anomaly-it’s a clinical liability.
my grandma took a generic blood pressure pill last month and it made her dizzy for three days. switched back to the brand and boom-back to normal. no one wants to pay more, but when your life’s on the line, you don’t gamble with crumbling tablets.
The FDA’s 57% failure rate for generic facilities is not surprising. The root cause is regulatory arbitrage: manufacturers locate production in countries with lax oversight, then export to the U.S. under the same label. The 2024 Drug Supply Chain Security Act is a band-aid. What’s needed is mandatory real-time batch traceability from raw material to patient, with blockchain-verified logs. Until then, we’re playing Russian roulette with our prescriptions. And don’t get me started on the fact that some generic manufacturers use the same excipients as industrial-grade pharmaceuticals-just repackaged.
People act like this is new. It’s not. The FDA’s been warning about this since 2012. The difference now is that more people are noticing because generics are everywhere. If you’re taking metformin or levothyroxine and suddenly feel off, it’s not ‘in your head.’ It’s the batch. Pharmacies don’t track manufacturer changes unless you ask. Demand lot numbers. Keep receipts. If your pill looks different, it probably is.
OH MY GOD. I KNEW IT. I KNEW IT. I’ve been saying this for YEARS! My cousin’s kid was on a generic seizure med and had THREE SEIZURES in one week because the tablet was crumbling! The pharmacist said ‘it’s the same active ingredient’-BULLSHIT. Active ingredient doesn’t mean the damn thing stays together! My blood pressure is rising just thinking about this. We need to BAN cheap generics from overseas and bring manufacturing BACK TO AMERICA. #MakePillsGreatAgain
Man, I’ve worked in a pharmacy for 12 years and this is the #1 reason patients come back angry. One batch of generic lisinopril? Crumbly as a cookie. Next batch? Looks perfect but makes people nauseous. We don’t even know which manufacturer we’re getting until the box arrives. The system is broken. We need to stop treating medicine like toilet paper.
It’s important to recognize that not all generics are created equal-some manufacturers have excellent track records. The issue isn’t the generic model itself, but the race to the bottom in pricing. If we incentivize quality over cost-through tiered reimbursement or public recognition programs-we can shift the market. Patients and providers need to be empowered to ask: ‘Who made this?’ and ‘What’s the lot number?’ Knowledge is the first step toward accountability.
There’s a philosophical tension here between accessibility and safety. Generics democratized medicine, yes-but at what cost? If we sacrifice consistency for affordability, are we not commodifying human health? The pill is meant to be a vessel of healing, not a casualty of supply chain economics. Perhaps the answer isn’t more regulation, but a redefinition of value: what is a life worth saving, and how much are we willing to pay for certainty?
Let’s be honest-this entire narrative is manufactured by Big Pharma to scare people away from generics and back to their overpriced monopolies. The FDA is complicit. Those ‘defects’? Mostly cosmetic. The bioequivalence standards are rigged. And the ‘adverse events’? Correlation isn’t causation. People report ‘it didn’t work’ because they were told generics are inferior. It’s placebo effect in reverse. The real threat? The erosion of trust in affordable medicine.
THIS IS A SCANDAL. A FULL-ON PHARMACEUTICAL NIGHTMARE. Imagine taking a pill that’s supposed to keep you alive-and it just… FALLS APART in your hand. Or worse-your body doesn’t absorb it because the coating is junk. People are dying quietly. No headlines. No lawsuits. Just a grandma on the floor, confused, because her ‘same’ pill didn’t work. And the corporations? They’re laughing all the way to the bank. We need a congressional hearing. We need a Netflix documentary. We need to burn the whole system down.
LOL. You think this is bad? Wait till you find out the same factories that make your generic Adderall also make cheap Chinese vape cartridges. Same machines. Same workers. Same ‘quality control’-which means a guy with a flashlight and a guess. The FDA doesn’t inspect these places. They get a photo and a PDF. I’ve seen the reports. The system is a joke. And you’re all just sitting here talking about ‘defects’ like it’s a car recall. This is people dying.
Big thanks for sharing this. Really eye-opening. 🙏 We need more transparency-patients deserve to know who made their meds. Let’s push for QR codes on pill bottles that link to batch reports. Maybe even a ‘trust score’ for manufacturers? 👍 #SafeMedicinesForAll