Explore how humidity, temperature, clothing, and hygiene drive fungal skin discoloration, with practical tips to recognise and prevent it.
Read MoreFungal Skin Conditions: Causes, Symptoms, and Treatment
When dealing with Fungal Skin Conditions, skin infections caused by fungi that affect the outer layers, hair, or nails. Also known as fungal skin infections, it covers a wide range of problems that most people encounter at some point. Dermatophytes, a group of fungi that feed on keratin and cause the most common skin infections. Also called tinea fungi are responsible for athlete's foot and ringworm, while Candida, yeast that thrives in warm, moist areas and can invade skin folds. Known as yeast infection often shows up as a red, itchy rash. Specific names like Athlete's Foot, tinea pedis, a dermatophyte infection of the feet. Also referred to as tinea pedis and Ringworm, tinea corporis, a circular rash caused by dermatophytes on the body. Sometimes called tinea corporis illustrate how diverse these conditions can be. Understanding each entity helps you spot the problem early and choose the right treatment.
What Triggers Fungal Skin Conditions?
Environmental factors fungal skin conditions are heavily influenced by. High humidity, excessive sweating, and tight clothing create a perfect breeding ground for dermatophytes and Candida. When skin stays damp for long periods, the fungi can colonize without resistance, leading to discoloration and itching. Poor foot hygiene, such as walking barefoot in public showers, directly increases the risk of athlete's foot, while shared towels or clothing can spread ringworm across families. Seasonal changes matter too—summer heat often spikes infection rates because sweat and warm surfaces boost fungal growth. Even indoor heating in winter can dry skin, causing micro‑tears that let fungi slip in. Recognizing these triggers lets you adjust daily habits, like wearing breathable socks or using powder in shoes, which can cut the odds of an outbreak dramatically.
Symptoms vary by the fungus involved but share common signals. Dermatophyte infections usually start as a red, scaly patch that may develop a raised border and a clear center—classic ringworm appearance. Athlete's foot often begins between the toes with a soggy, itchy feel, then spreads to the soles. Candida infections favor skin folds, producing a moist, red rash that may ooze. Itching, burning, and occasional swelling are typical, and in severe cases, blisters or crusts appear. Because many skin issues look alike, a proper diagnosis often requires a visual exam and sometimes a lab sample. Early identification prevents the infection from spreading to other body parts or to other people.
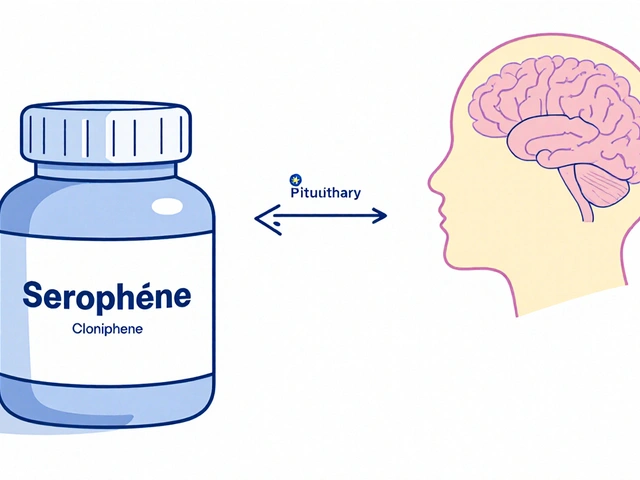
Treatment options target the specific fungus and the severity of the infection. Over‑the‑counter topical creams containing clotrimazole, terbinafine, or miconazole work well for mild dermatophyte cases and most Candida rashes. For stubborn or extensive infections, doctors may prescribe oral antifungals like fluconazole or itraconazole, which reach deeper skin layers. Alongside medication, lifestyle tweaks—keeping skin dry, changing socks daily, and avoiding tight shoes—support recovery and lower recurrence. In addition, disinfecting shared items (e.g., gym mats, nail clippers) breaks the infection chain. When you combine proper drug therapy with preventive habits, you usually clear the infection within a few weeks and keep it from coming back.
Below you’ll find a curated set of articles that dive deeper into each of these topics. From environmental triggers to medication comparisons, the collection offers practical advice, real‑world comparisons, and up‑to‑date safety tips to help you manage any fungal skin condition you might face.