Fertility Treatment Decision Calculator
Find Your Best Fertility Treatment Option
Answer a few simple questions to see which fertility medication might be most appropriate for you based on your unique situation.
Quick Takeaways
- Serophene (Clomiphene) is a selective estrogen receptor modulator most often used as first‑line ovulation induction.
- Letrozole, an aromatase inhibitor, offers slightly higher live‑birth rates for women with PCOS.
- Gonadotropins give the highest ovulation success but cost significantly more and need injections.
- Side‑effect profiles differ: clomiphene can cause hot flashes and visual disturbances, while letrozole’s main issues are mild fatigue and joint pain.
- Choosing the right drug depends on diagnosis, age, BMI, previous cycles and budget.
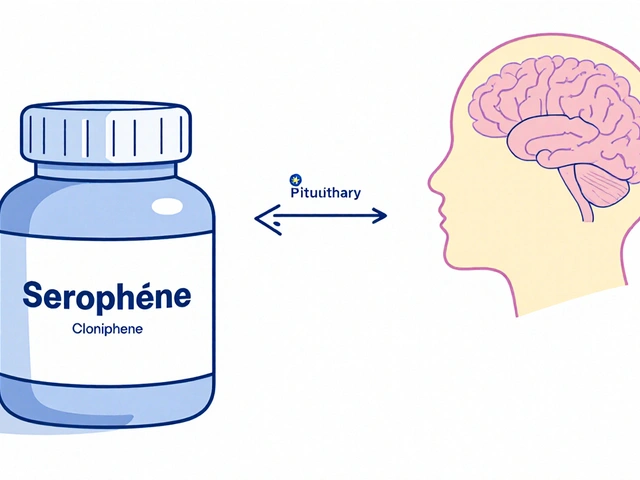
When a woman’s doctor recommends a fertility pill, the first question is usually “Is Serophene the best option for me?” Below we break down how Serophene (the brand name for Clomiphene citrate is a selective estrogen receptor modulator (SERM) that triggers ovulation by blocking estrogen feedback in the hypothalamus) measures up against the most common alternatives. The goal is to give you a clear picture of mechanisms, success rates, side effects, cost and practical considerations so you can decide with confidence.
How Serophene Works and Who It’s Typically Prescribed For
Serophene belongs to the SERM class. By binding estrogen receptors in the hypothalamus, it tricks the brain into thinking estrogen levels are low. The pituitary gland then releases more follicle‑stimulating hormone (FSH), prompting a follicle to mature and release an egg. It’s usually started on day 3‑5 of the menstrual cycle, with doses ranging from 25 mg to 150 mg per day for five days.
Typical candidates include:
- Women with anovulatory cycles due to hypothalamic dysfunction.
- Patients with mild polycystic ovary syndrome (PCOS) who haven’t responded to lifestyle changes.
- Those seeking an oral, non‑injectable first‑line option.
Top Alternatives at a Glance
While Serophene has been a staple for decades, newer agents and injectable hormones have entered the scene. Here’s a snapshot of the most relevant alternatives:
- Letrozole - an aromatase inhibitor that lowers estrogen production, indirectly increasing FSH release.
- Tamoxifen - another SERM, less commonly used for fertility but occasionally considered when clomiphene fails.
- Gonadotropins - injectable FSH (often as Menotropin) that directly stimulates the ovaries.
- Anastrozole - a newer aromatase inhibitor with limited fertility data.
- Metformin - an insulin‑sensitizer used off‑label for PCOS‑related ovulation issues.
Decision Criteria: What to Compare
Before diving into numbers, think about the factors that matter most to you:
- Mechanism of action - does the drug fit your hormonal profile?
- Ovulation and live‑birth success rates - raw percentages from recent meta‑analyses.
- Side‑effect burden - both frequency and severity.
- Cost and insurance coverage - especially important in the UK where NHS prescribing varies.
- Convenience - oral pill vs injection, monitoring requirements.
Side‑by‑Side Comparison Table
| Drug | Mechanism | Typical Dose | Ovulation Rate | Live‑Birth Rate | Common Side‑effects | Average Cost per Cycle (GBP) |
|---|---|---|---|---|---|---|
| Serophene (Clomiphene) | SERM - blocks estrogen feedback | 25‑150 mg PO daily for 5 days | ≈78 % (per cycle) | ≈28 % (per cycle) | Hot flashes, visual disturbances, ovarian cysts | £30‑£45 |
| Letrozole | Aromatase inhibitor - reduces estrogen synthesis | 2.5‑7.5 mg PO daily for 5 days | ≈84 % (PCOS groups) | ≈31 % (per cycle) | Mild fatigue, joint pain, occasional nausea | £35‑£50 (often off‑label prescribed) |
| Tamoxifen | SERM - similar to clomiphene but weaker | 20‑40 mg PO daily for 5 days | ≈65 % (limited studies) | ≈22 % (per cycle) | Vaginal dryness, hot flashes | £25‑£40 |
| Gonadotropins (Menotropin) | Injectable FSH - directly stimulates follicular growth | 75‑150 IU SC daily, 5‑10 days | ≈92 % (with monitoring) | ≈38 % (per cycle) | Multiple‑pregnancy risk, injection site pain, OHSS | £500‑£900 |
| Metformin (adjunct) | Insulin sensitizer - improves ovulatory response | 500‑1500 mg PO daily | ≈70 % when combined with clomiphene | ≈25 % (when used with clomiphene) | GI upset, metallic taste | £15‑£30 |
Deep Dive: When to Choose Serophene
Serophene remains a solid first‑line choice for many reasons:
- Affordability: At under £50 per cycle, it’s the most cost‑effective option on the UK market.
- Oral convenience: No injections, no daily ultrasounds (unless you’re a high‑risk patient).
- Well‑studied safety profile: Over 40 years of data, with rare serious adverse events.
- Predictable dosing: Simple 5‑day regimen works for most women under 35 with normal BMI.
However, it has a few drawbacks that push clinicians toward alternatives:
- Resistance: About 10‑15 % of patients develop clomiphene resistance after three failed cycles.
- Thickened endometrium: In some cases, the drug’s anti‑estrogen effect can thin the lining, harming implantation.
- Multiple‑pregnancy risk: Although lower than with gonadotropins, the risk is still present (≈5‑7 %).
Letrozole: The Rising Contender, Especially for PCOS
Letrozole’s popularity surged after several RCTs showed a modest but statistically significant edge in live‑birth rates for women with PCOS. Because it lowers estrogen rather than blocks its receptors, the endometrium usually stays more receptive.
Key points when considering letrozole:
- Shorter half‑life: Less lingering estrogen suppression, which can reduce side‑effects.
- Lower triple‑dose requirement: Most protocols use 2.5‑5 mg for three to five days.
- Fewer visual disturbances: Patients report fewer “spotting” visual flips than with clomiphene.
On the flip side, letrozole is technically an off‑label use for fertility in the UK, so some NHS trusts may need a specialist’s justification for prescribing.
Injectable Gonadotropins: When Maximum Power Is Needed
If you’ve tried oral agents without success, gonadotropins are the next step. By delivering FSH directly, they bypass the hypothalamic‑pituitary axis entirely. The result is the highest ovulation and live‑birth rates, but the price tag and monitoring workload rise steeply.
Factors to weigh:
- Monitoring intensity: Requires serial transvaginal ultrasounds and serum estradiol checks to avoid ovarian hyperstimulation syndrome (OHSS).
- Multiple pregnancy risk: Up to 20 % of cycles result in twins or higher-order multiples.
- Insurance coverage: Some private insurers cover part of the cost, but NHS provision is usually limited to specific cases.

Special Situations: PCOS, High BMI, and Age Over 35
Women with polycystic ovary syndrome often have insulin resistance. Adding Metformin can improve clomiphene responsiveness by up to 15 %. For those with a BMI above 30, letrozole tends to be more effective than clomiphene because obesity can blunt estrogen‑feedback mechanisms.
Age is another decisive factor. Women over 35 have a reduced ovarian reserve, so many clinics move directly to gonadotropins or even IVF after one failed oral cycle.
Practical Checklist Before Your Next Appointment
- Confirm your exact diagnosis (PCOS, unexplained infertility, hypogonadotropic amenorrhea).
- Know your baseline BMI and recent hormonal panel (FSH, LH, AMH).
- Ask about NHS coverage for each drug - serophene is usually listed, letrozole may need a specialist letter.
- Prepare a list of previous cycle outcomes (dose, side‑effects, ovulation confirmation).
- Discuss the possibility of combination therapy (e.g., clomiphene + metformin) if you’ve had partial success.
Bottom Line: Mapping the Right Path
In a nutshell, Serophene (Clomiphene) is still the go‑to first‑line oral agent for many women because it’s cheap, simple and well‑studied. Letrozole provides a modest bump in live‑birth rates for PCOS and carries fewer estrogen‑related side effects. Gonadotropins deliver the highest success but at a far greater cost and monitoring burden.
Ask yourself:
- Do I need the cheapest, easiest option? → Serophene.
- Do I have PCOS and want a slightly higher chance? → Letrozole (maybe with Metformin).
- Have I failed multiple oral cycles or need the fastest route to pregnancy? → Gonadotropins.
Whatever you choose, keep open communication with your fertility specialist and monitor how your body reacts. The right drug paired with the right timing can turn a hopeful plan into a real pregnancy.
Frequently Asked Questions
Can I switch from Serophene to Letrozole mid‑cycle?
No. Both drugs act on the same hormonal window, so they must be started on day 3‑5 of a fresh menstrual cycle. Switching mid‑cycle can cause unpredictable hormone spikes and lower ovulation chances.
What is "clomiphene resistance" and how is it managed?
Resistance means you’ve had three or more full‑dose cycles without ovulation. Doctors usually try a higher dose, add Metformin, or move to Letrozole or gonadotropins.
Is it safe to use Serophene if I have a thyroid disorder?
Generally yes, but uncontrolled thyroid disease can affect ovulation. Make sure your thyroid‑stimulating hormone (TSH) is within target range before starting any fertility drug.
How many cycles should I try before considering IVF?
Most clinics recommend three full cycles of an oral agent (or two if you move to gonadotropins). After that, if pregnancy hasn’t occurred, many specialists discuss IVF as the next step.
Do NHS prescriptions cover the cost of Letrozole for fertility?
Only in cases where a specialist provides a written justification that clomiphene has failed. Otherwise patients usually pay privately.



10 Comments
Oh great, another pill showdown, because we needed more options.
Seriously, the price gap between Serophene and Letrozole is ridiculous. In India we see patients struggling to afford the cheapest option, let alone the cost‑heavy gonadotropins. The NHS list price makes no sense when the real out‑of‑pocket expense can be five times higher. It feels like the pharma companies are playing a game of who can charge the most for a tiny hormonal tweak.
Alright, buckle up because we need to talk about the sheer nightmare that is the “clomiphene resistance” myth. You see, the literature loves to throw around the term like it’s a badge of honor, yet it’s really just a signal that the body’s feedback loop is being messed up by a drug that was invented decades ago. First, the dosage buffer is absurd – doctors start at 25 mg and then jump to 150 mg, as if the ovaries have a volume knob. Second, the visual disturbances aren’t just occasional flickers; they’re real migraines that can ruin a day. Third, the ovarian cyst formation rate is non‑trivial and can lead to painful interventions. Fourth, the endometrial thinning effect can sabotage implantation after you finally get that egg out. Fifth, the hormone surge from clomiphene can actually make the pituitary more resistant over time, creating a vicious cycle. Sixth, patient compliance drops because the side‑effects feel like a sequel to chemotherapy. Seventh, the cost‑benefit analysis often ignores the downstream expenses of extra ultrasounds and blood tests. Eighth, the data on live‑birth improvement for Letrozole in PCOS is consistently better across multiple meta‑analyses. Ninth, the off‑label status of Letrozole is a bureaucratic hurdle, but the clinical outcomes speak louder than paperwork. Tenth, combining clomiphene with Metformin gives a marginal boost, but it’s still not a game‑changer. Eleventh, many clinics still push clomiphene because it’s cheap and they get reimbursed easily. Twelfth, the emotional toll on couples who endure multiple failed cycles is massive, often leading to depression. Thirteenth, the risk of multiple pregnancies, while lower than gonadotropins, is still present and can result in high‑risk deliveries. Fourteenth, the lack of individualized dosing protocols means a lot of patients are stuck in a one‑size‑fits‑all approach. Fifteenth, the cultural stigma around fertility drugs can keep women from seeking help early. Finally, the bottom line is that the industry is stuck in a loop of pushing an older drug while newer, more effective options get sidelined by red tape and cost barriers.
The mechanisms described are accurate and the comparative data aligns with recent studies.
While the science is solid, we must also consider the ethical dimension of prescribing expensive treatments without clear insurance coverage. It is unjust to burden patients financially when cheaper alternatives exist. Healthcare equity demands transparency and patient‑centered decision making.
I appreciate the overview and would add that monitoring protocols can be streamlined to reduce clinic visits, benefiting both patients and providers.
Wow, this is like a roller‑coaster of hormones! 🎢💊 I’m feeling all the drama of choosing between cheap pills and pricey shots. The side‑effects sound like a soap‑opera plot twist, and the cost numbers are enough to make anyone’s wallet cry. Let’s hope everyone finds the perfect match for their journey! 🌈✨
Great summary, keep the optimism flowing.
The table makes it clear which drug fits which situation based on cost and success rates.
Exactly! And remember that the emotional rollercoaster can be just as taxing as the financial one. Staying positive and having a support system makes a huge difference; keep cheering each other on and don’t forget to celebrate the small wins along the way!