Every year, hundreds of thousands of patients in U.S. hospitals suffer harm because of preventable medication errors. These aren’t rare accidents-they’re systemic failures that happen because of tiny oversights: a misplaced decimal, a misread label, a rushed check. The good news? We know how to stop them. The bad news? Too many hospitals still aren’t doing it right.
What Medication Safety Really Means
Medication safety isn’t just about giving the right drug. It’s about making sure the right drug gets to the right patient, at the right time, in the right dose, through the right route-every single time. The American Society of Health-System Pharmacists defines it as preventing any event that could lead to inappropriate use or patient harm while the medication is under care of a healthcare provider. This isn’t theoretical. In 1999, the Institute of Medicine found that between 44,000 and 98,000 people die each year in U.S. hospitals from preventable medical errors. About 7,000 of those deaths are tied to medication mistakes. That’s more than car accidents. And it’s not just deaths-studies show at least one medication error happens per hospital patient every day. In 2026, we still see 400,000 preventable drug-related injuries in hospitals annually. The cost? Around $21 billion a year in the U.S. alone. That’s not just money-it’s lost time, broken trust, and lives changed.The ISMP Targeted Best Practices: What Works
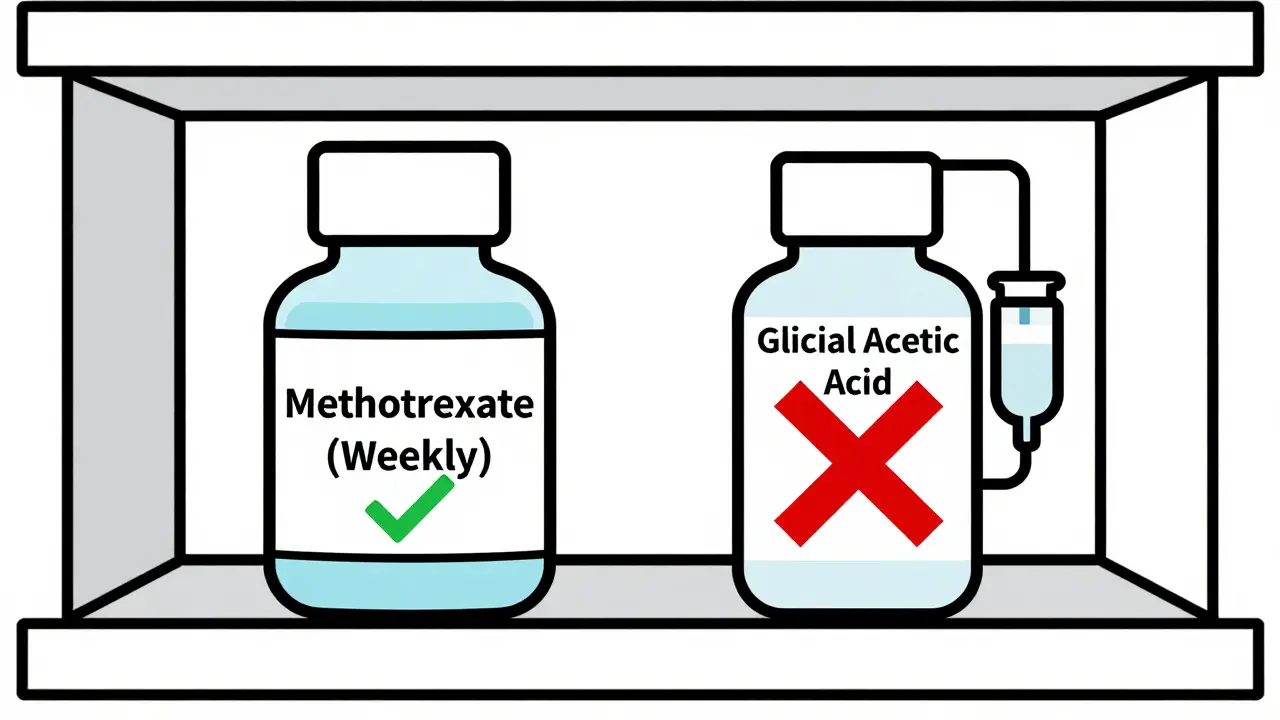
The Institute for Safe Medication Practices (ISMP) released its Targeted Medication Safety Best Practices for Hospitals in 2014, with the latest update in 2020-2021. It’s not a suggestion list-it’s a playbook built from real error reports submitted by frontline staff. There are 19 specific practices, and each targets a high-risk scenario that’s caused real harm. One of the most powerful? Preventing daily dosing of methotrexate. This drug is used weekly for autoimmune diseases and cancer. If given daily by mistake, it can kill a patient in days. The ISMP rule requires three things:- Electronic systems must default to weekly dosing
- Any daily order triggers a hard stop-clinicians must confirm it’s for cancer treatment
- Patients get both written and verbal instructions before discharge, including a printed list they must double-check
High-Alert Medications: The Big Risks
Some drugs are just more dangerous. The ISMP and ASHP lists include insulin, opioids, anticoagulants, IV potassium, and neuromuscular blocking agents. These aren’t just high-risk-they’re high-stakes. One wrong dose can paralyze, stop a heart, or cause irreversible brain damage. Hospitals that follow ASHP guidelines use three layers of protection:- Prevent errors: Standardized concentrations (e.g., all IV heparin is 100 units/mL, not 10 or 1,000)
- Make errors visible: Barcode scanning at the bedside so the system checks patient ID, drug, dose, and timing
- Mitigate harm: Independent double-checks for high-alert drugs-two licensed staff verify before giving
Technology That Saves Lives
Barcode medication administration (BCMA) systems are now standard in most large hospitals. A 2022 AHRQ report shows 89% of hospitals with 300+ beds use them. Only 54% of smaller hospitals do. Why? Cost. Training. Legacy EHR systems that won’t integrate. But BCMA isn’t magic. It only works if:- The barcode on the drug matches the order
- The patient’s wristband is scanned
- The nurse scans their own ID
- The system confirms the right time and route
Where the System Breaks Down
The biggest problems aren’t in the pharmacy. They’re in the chaos of daily care. A nurse manager in a rural hospital posted on the American Nurses Association board that the requirement for dual verbal and written methotrexate discharge instructions created bottlenecks during staffing shortages. She had one pharmacist for 120 patients. She couldn’t do both. So she did one-and risked a gap. Another issue? Electronic health records (EHRs). A 2021 ASHP survey found 63% of hospitals struggled to build hard stops because their EHR vendor wouldn’t customize the system. Some hospitals worked around it by having pharmacists manually review every high-risk order until upgrades were approved. That’s a band-aid on a bullet wound. And then there’s culture. A Reddit post from an ICU nurse described a case where a neuromuscular blocker was given without a double-check. The system had the alert. The pharmacist flagged it. But the doctor insisted, and the nurse didn’t push back. “We were told not to question orders,” she wrote. “That’s how people die.”What Patients Can Do
You’re not powerless. A 2022 National Council on Aging survey found 68% of adults over 65 felt safer when hospitals verified their identity with name, birth date, and wristband before giving any medication. Here’s what you can do:- Ask: “Is this the right drug for me?”
- Check your discharge papers against what you’re told
- Bring a list of all your meds-even supplements-to every appointment
- If you’re given a new drug, ask: “What’s this for? What are the side effects? What should I do if I feel something’s wrong?”
What’s Changing in 2026
The field is evolving fast. In 2023, ISMP added new rules for compounded sterile preparations after a fungal meningitis outbreak killed 76 people. The FDA now requires clearer labeling for high-concentration electrolytes like potassium chloride-full compliance is due by December 31, 2024. The AHRQ’s 2023 National Action Plan aims to cut opioid-related harm by 50% by 2027. Meanwhile, Gartner predicts 75% of U.S. hospitals will use AI to detect medication errors in real time by 2025. Right now, only 22% do. And ISMP is expanding its Best Practices to outpatient clinics in 2024-2025. Why? Because medication errors are rising there too. Between 2018 and 2022, outpatient errors jumped 47%. More people are getting prescriptions from urgent care centers, telehealth visits, and retail clinics-and fewer safety nets exist.Why This Matters Everywhere
Medication safety isn’t just a hospital problem. It’s a clinic problem. A pharmacy problem. A patient problem. The systems that work in a 1,000-bed academic center often don’t scale to a 50-bed rural clinic. But the risks are the same. The solution isn’t more rules. It’s smarter systems, better training, and a culture where anyone-nurse, pharmacist, patient-feels safe speaking up. The data proves it: when hard stops, barcode scans, and double-checks are used together, harm drops. Fast. The question isn’t whether you can afford to fix this. It’s whether you can afford not to.What is the most common cause of medication errors in hospitals?
The most common cause is miscommunication-between prescribers, pharmacists, and nurses. This includes unclear handwriting on paper orders, misread abbreviations (like “U” for units instead of “unit”), and rushed handoffs during shift changes. Electronic systems have reduced this, but 63% of hospitals still struggle to customize their EHRs to prevent these errors.
Are all hospitals required to follow ISMP best practices?
No. ISMP’s Targeted Best Practices are voluntary guidelines, not federal law. However, the Joint Commission and CMS tie accreditation and reimbursement to medication safety performance. Hospitals that ignore these practices risk losing funding or accreditation. Most large hospitals follow them because the evidence is clear: they save lives and money.
What are high-alert medications, and why are they dangerous?
High-alert medications have a higher risk of causing serious harm if used incorrectly. Examples include insulin, opioids, anticoagulants, IV potassium, and neuromuscular blockers. A small mistake-like giving 10 times the dose of insulin or confusing a paralytic with a sedative-can lead to death or permanent injury. That’s why they require extra safeguards: standardized concentrations, double-checks, and hard stops in electronic systems.
How effective are barcode scanning systems in preventing errors?
Barcode scanning reduces medication errors by 41-86%, according to multiple studies. But effectiveness depends on consistent use. If staff skip scanning because they’re rushed or the scanner is broken, the system fails. The best results come when scanning is mandatory, integrated into workflow, and supported by training-not treated as a checkbox.
Can patients really help prevent medication errors?
Yes. Studies show patients who ask questions, bring a medication list, and verify their identity before receiving drugs reduce their risk of error by up to 40%. Hospitals that encourage patient involvement-like requiring name and birth date checks before giving any drug-see fewer mistakes. Your voice matters.
Why are smaller hospitals falling behind in medication safety?
Smaller hospitals often lack the budget for modern EHRs, barcode systems, and dedicated pharmacists. Staff shortages make it hard to implement double-checks. Vendor software may not support custom safety rules. And without the resources to train staff or track errors, they rely on older, riskier methods. The result? A dangerous gap in safety between urban and rural care.





