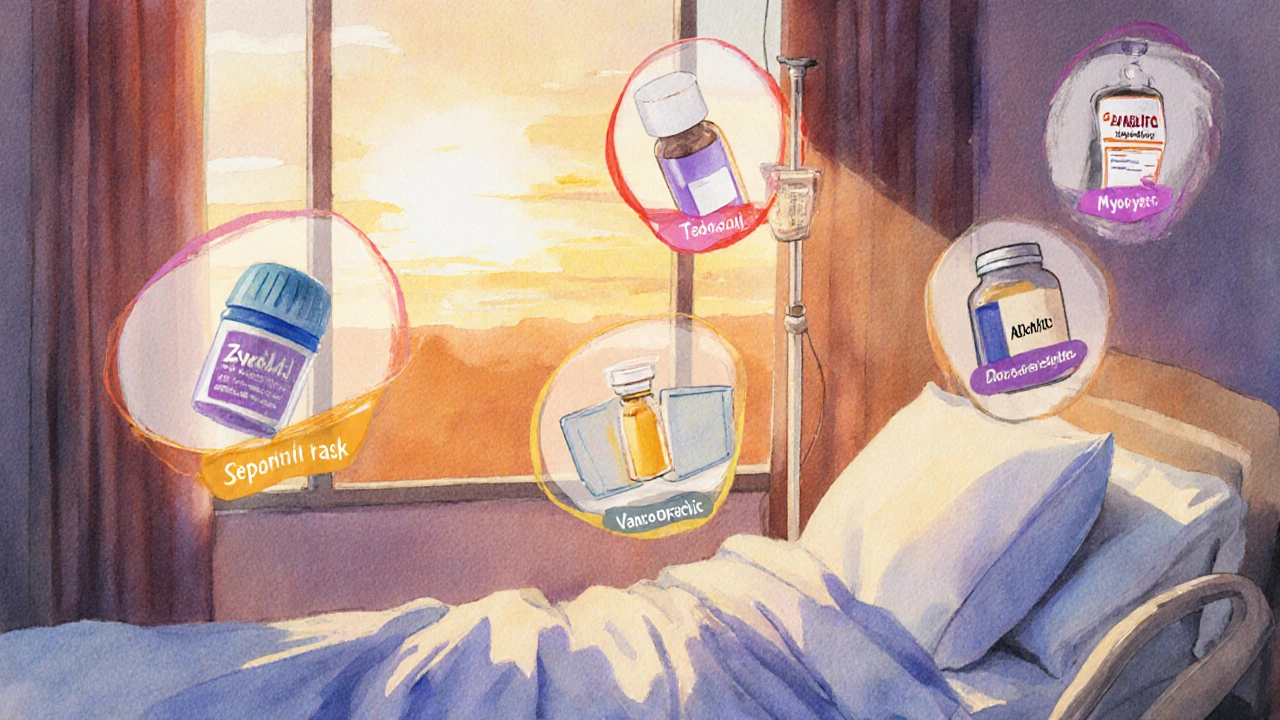
Zyvox vs Alternatives: Treatment Decision Helper
Recommended Treatment
Zyvox (Linezolid)
Excellent lung penetration, broad spectrum, oral availability
Hematologic risk Serotonin syndrome riskTedizolid
Shorter course, fewer hematologic effects
Less GI upset Newer agentDaptomycin
Best for bacteremia, no renal impact
Myopathy risk IV onlyVancomycin
Lowest cost, requires monitoring
Nephrotoxicity OtotoxicityTL;DR
- Zyvox (linezolid) is an oral/IV oxazolidinone used for MRSA and VRE infections.
- Key alternatives include tedizolid, daptomycin, vancomycin and newer oxazolidinones.
- Linezolid offers excellent lung penetration but carries a risk of serotonin‑syndrome and blood‑count suppression.
- Tedizolid has a shorter course and fewer hematologic side‑effects, while daptomycin is preferred for bacteremia.
- Cost, route of administration, and infection site drive the final choice.
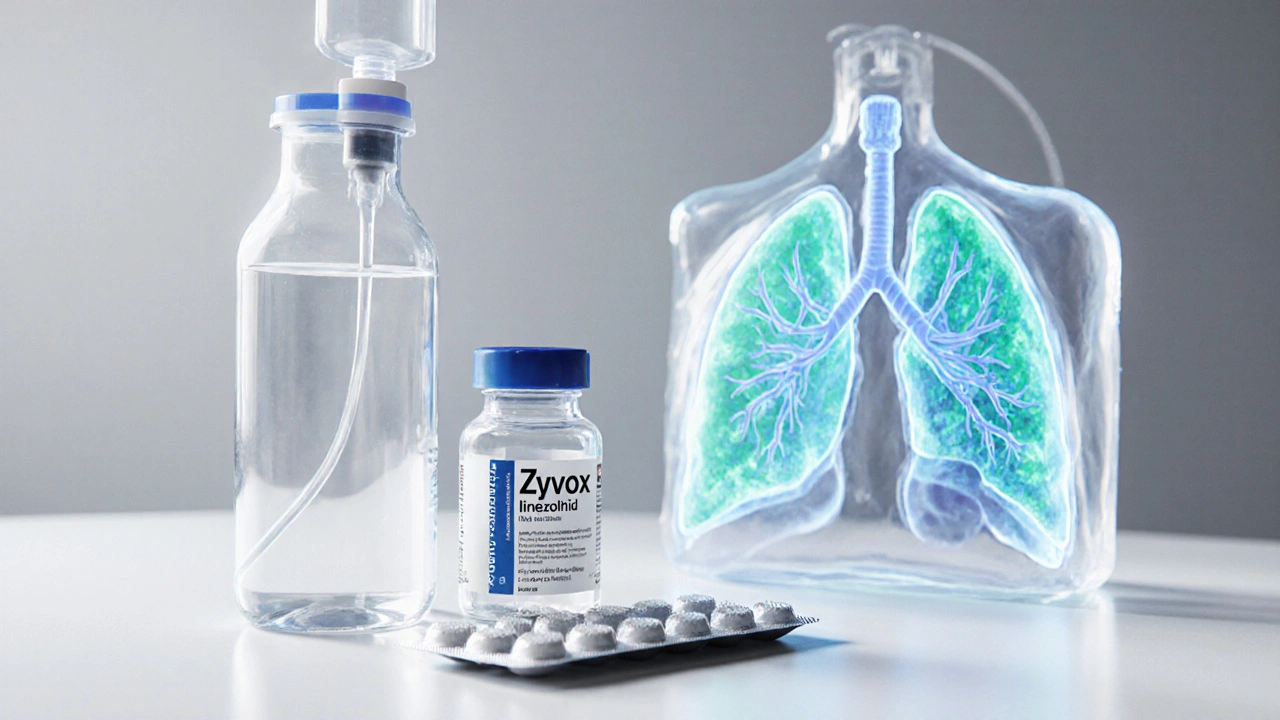
What is Zyvox?
When you see Zyvox on a prescription label, you’re looking at a branded form of linezolid, a synthetic antibiotic that belongs to the oxazolidinone class. First approved by the FDA in 2000, linezolid was a game‑changer because it works against Gram‑positive bacteria that resist many other drugs, especially MRSA (methicillin‑resistant Staphylococcus aureus) and VRE (vancomycin‑resistant Enterococcus).
How Zyvox Works
Linezolid inhibits protein synthesis by binding to the 50S ribosomal subunit. This stops bacteria from making essential proteins, leading to a bacteriostatic effect in most strains. Because the drug reaches high concentrations in lung tissue, it’s especially useful for pneumonia caused by resistant organisms.
Key Benefits of Zyvox
- Available both intravenously and orally - you can switch to pills without losing efficacy.
- Excellent penetration into the epithelial lining fluid of the lungs.
- Broad activity against most Gram‑positive pathogens, including those resistant to beta‑lactams.
- Can be used for skin‑and‑soft‑tissue infections, bone infections, and certain prosthetic‑joint infections.
Common Side Effects and Safety Concerns
The most talked‑about risks are hematologic. Linezolid can suppress bone‑marrow production, leading to thrombocytopenia, anemia or neutropenia, especially after more than two weeks of use. It also inhibits monoamine oxidase, so patients on SSRIs, SNRIs, or certain pain meds can develop serotonin syndrome.
Other frequent complaints include headache, nausea, diarrhoea, and a metallic taste. Because it’s metabolised in the liver, patients with severe hepatic impairment need dose adjustments.

Typical Dosing Regimens
- Adults: 600mg every 12hours, either IV or oral.
- Kidney impairment: No adjustment needed unless on dialysis, where a 24‑hour window after the dose is recommended.
- Children (12kg‑12yr): 10mg/kg every 12hours, maximum 600mg.
Therapeutic drug monitoring isn’t routine, but some clinicians check trough levels when treatment exceeds 14days to avoid toxicity.
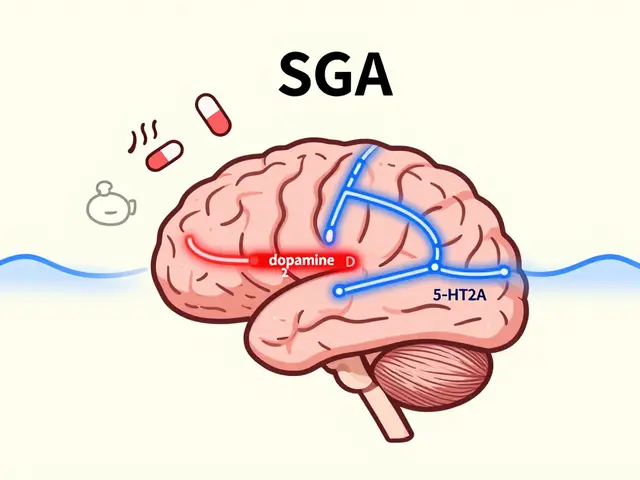
Alternative Oxazolidinones and Other Antibiotics
While linezolid remains a workhorse, a handful of other agents compete for the same market slice. Below is a quick snapshot of each.
| Attribute | Zyvox (Linezolid) | Tedizolid | Daptomycin | Vancomycin |
|---|---|---|---|---|
| Drug class | Oxazolidinone | Oxazolidinone | Lipopeptide | Glycopeptide |
| Typical route | IV & PO | IV & PO | IV only | IV only |
| Indications (major) | MRSA, VRE, pneumonia, skin/soft‑tissue | ABSSSI, nosocomial pneumonia | Bacteremia, endocarditis, skin infections | MRSA, C.diff. colitis (oral), pneumonia |
| Course length | 10‑14days (standard) | 6‑10days (shorter) | 7‑14days (depends on infection) | 7‑14days (often longer) |
| Key safety concerns | Hematologic, serotonin syndrome | Less thrombocytopenia, mild GI | Myopathy (CK rise), eosinophilia | Nephrotoxicity, ototoxicity |
| Cost (US, 2025) | ~$250/day (IV), $120/day (PO) | ~$180/day (IV), $100/day (PO) | ~$200/day | ~$40-$70/day |
When to Choose Zyvox Over Others
If you need an oral option that still reaches high lung concentrations, linezolid is usually the front‑runner. It shines in two scenarios:
- Hospital‑acquired or ventilator‑associated pneumonia caused by MRSA or VRE - the drug’s lung penetration beats daptomycin (which is inactivated by surfactant).
- Patients who can’t tolerate vancomycin because of kidney issues; linezolid bypasses the kidneys.
However, if the infection is a bloodstream infection without a lung component, daptomycin or vancomycin may be safer, especially for prolonged therapy where linezolid’s blood‑count effects become problematic.
Safety, Drug Interactions, and Special Populations
Because linezolid is a reversible monoamine‑oxidase inhibitor (MAOI), you must check any concurrent serotonergic meds. A quick rule of thumb: avoid SSRIs, tramadol, meperidine, and St.John’s wort unless you switch or monitor closely.
Pregnant or breastfeeding mothers should only use linezolid if the benefit outweighs risk; animal studies show some fetal toxicity, and it crosses the placenta.
Elderly patients often have reduced marrow reserve, so routine CBC monitoring weekly after day7 is prudent.
Cost and Accessibility Considerations
In the UK, Zyvox is a prescription‑only medicine listed on the NHS formulary under the brand name Zyvox. The price difference between IV and oral formulations can affect hospital budgets. Generic linezolid is available, cutting the daily cost by roughly 40%.
Tedizolid’s generic version entered the market in early 2024, making it a cheaper 6‑day course for skin infections. Daptomycin remains pricey, while vancomycin is the most affordable but requires therapeutic drug monitoring.
Quick Decision Checklist
- Is the infection primarily lung‑based? → Favor linezolid or tedizolid.
- Do you need an IV‑only regimen? → Consider daptomycin or vancomycin.
- Is the patient on serotonergic drugs? → Avoid linezolid.
- Is renal function compromised? → Linezolid or tedizolid are safer than vancomycin.
- Are you treating a bloodstream infection? → Daptomycin is preferred.
- Budget constraints? → Vancomycin is cheapest; generic linezolid offers a middle ground.
Frequently Asked Questions
Can I switch from IV to oral linezolid mid‑treatment?
Yes. One of linezolid’s biggest advantages is its 100% oral bioavailability, so you can safely step down to pills once the patient is stable, without losing drug exposure.
How does tedizolid differ from linezolid?
Tedizolid is a newer oxazolidinone that requires a 200mg once‑daily dose for 6days (vs 600mg twice daily for 10‑14days). It causes less thrombocytopenia and has a lower risk of serotonin syndrome, making it attractive for patients on antidepressants.
Is linezolid effective against Gram‑negative bacteria?
No. Linezolid’s activity is limited to Gram‑positive organisms. For Gram‑negative infections you need a different class, such as carbapenems or fluoroquinolones.
What monitoring is required during a 2‑week linezolid course?
Baseline CBC, then weekly CBCs to catch dropping platelets or neutrophils. Also check for peripheral neuropathy if therapy exceeds 28days.
Why does vancomycin cost less than linezolid in the UK?
Vancomycin has been generic for decades, and the NHS pricing contracts secure low per‑dose rates. Linezolid is newer, patented (though generic versions exist), and requires more expensive production processes, especially for the IV formulation.



13 Comments
The mechanistic underpinnings of linezolid's oxazolidinone class confer a unique inhibition of the 50S ribosomal subunit, thereby arresting bacterial protein synthesis. Its pharmacokinetic profile, characterized by near‑complete oral bioavailability, renders it a formidable contender in the armamentarium against multidrug‑resistant Gram‑positive pathogens. When juxtaposed with tedizolid, one must consider the augmented risk of thrombocytopenia inherent to prolonged linezolid exposure, a phenomenon attributable to mitochondrial protein synthesis perturbation. Moreover, the monoamine‑oxidase inhibitory activity precipitates a non‑trivial serotonin syndrome risk in patients concomitantly prescribed serotonergic agents. From a cost‑effectiveness perspective, generic linezolid formulations have narrowed the fiscal chasm relative to vancomycin, yet remain superiorly priced only to a limited extent. Clinicians should vigilantly monitor complete blood counts weekly after the seventh day of therapy to mitigate hematologic sequelae. Ultimately, the decision matrix must integrate infection locus, renal function, and drug interaction potential to optimize therapeutic outcomes.
Great overview! If you’re looking for a simple way to decide, think about whether the patient can take pills and if they’re on any antidepressants. For lung infections, linezolid works well, but keep an eye on blood counts. If cost is a big factor, vancomycin is cheaper but needs blood level checks.
Watch blood counts weekly.
Imagine standing at the crossroads of antimicrobial stewardship, where each decision reverberates through the microbiome like a pebble rippling across a pond. Linezolid, with its impressive lung penetration, beckons the clinician toward the horizon of oral convenience, yet it also whispers warnings of marrow suppression, a silent sentinel that may awaken after weeks of therapy. The alternative, tedizolid, arrives on a shorter runway, demanding fewer days and offering a gentler touch on platelets, a subtle nod to patient safety. Meanwhile, daptomycin strides confidently into the bloodstream battlefield, immune to the surfactant‑mediated inactivation that haunts linezolid in pneumonia, though it demands the exclusivity of IV administration and obliges the clinician to monitor creatine kinase. Vancomycin, the veteran, stands resilient on the cost‑effectiveness front, yet it exacts a toll of renal monitoring and potential ototoxicity. In the grand calculus, renal function emerges as a pivotal variable: patients with impaired kidneys may find linezolid or tedizolid more forgiving, while those with intact function can tolerate vancomycin’s nephrotoxic shadows. Serotonergic medication use, too, casts a decisive shade; the MAO‑inhibitory nature of linezolid necessitates a careful withdrawal or substitution strategy to avert serotonin syndrome. Cost, of course, is the ever‑present undercurrent, with generic linezolid narrowing the price gap but still trailing behind vancomycin’s modest daily expense. When we synthesize these strands-site of infection, route preference, comorbidities, drug interactions, and budgetary constraints-we arrive at a nuanced tapestry rather than a single‑threaded directive. Thus, the clinician’s role transforms from a mere prescriber to a strategic architect, weaving together pharmacologic virtues and patient‑specific factors into a coherent, individualized therapeutic plan.
Linezolid is good for lungs 👍 but watch those blood counts 😬 and avoid SSRIs 🚫💊
Consider, if you will, the intricate tapestry of antimicrobial selection; linezolid offers, undeniably, a commendable oral bioavailability, yet it is not without its caveats-hematologic suppression, serotonin syndrome, and the inexorable rise in treatment‑associated costs; tedizolid, conversely, presents a truncated therapeutic course, fewer hematologic perturbations, and a comparable spectrum of activity, thereby positioning itself as a logical alternative when the clinician wishes to mitigate adverse events; daptomycin, however, remains steadfastly reserved for bacteremia, its inability to traverse the pulmonary surfactant rendering it ineffective in pneumonia, whilst vancomycin maintains its status as a cost‑effective, albeit nephrotoxic, mainstay-thus, the decision tree diverges based upon renal function, infection locus, concomitant serotonergic agents, and economic considerations.
Ah, the eternal dance between efficacy and expense-linezolid dazzles with oral convenience, yet one must gently remind the patient that the price tag is not merely decorative. If the kidneys are whispering distress, perhaps a retreat to vancomycin, with its humble cost, is the pragmatic bow. Of course, if the patient is already juggling a serotonin‑reuptake inhibitor, a polite nod to tedizolid might spare the drama of serotonin syndrome. Indeed, the art lies in balancing pharmacology with the patient’s fiscal reality.
When you break it down, linezolid is the Swiss‑army knife of Gram‑positive coverage – portable, versatile, and with that sweet lung penetration. But remember, it’s not a free lunch; the blood counts can take a hit after a couple weeks. On the flip side, tedizolid is the sleek, newer model – shorter course, fewer platelet worries, still good for lungs. If you need a pure IV hero for bloodstream infections, daptomycin steps into the ring, though it won’t help with pneumonia because the surfactant knocks it out. And then there’s the old faithful vancomycin – cheap, but you’ll be chasing kidney labs. So, match the drug to infection site, patient meds, and budget, and you’ll have a winning combo.
Honestly linezolid is overrated, cheap versions are fine but the hype about oral switch is just marketing and the blood count thing is a nightmare
Hey folks! 🌟 If you’ve got a patient battling a tough lung infection, linezolid shines like a bright sunrise – you can take it by mouth and still hit the bugs hard. Just keep an eye on those platelets, and if the patient’s on antidepressants, consider tedizolid for a smoother ride. For bloodstream battles, daptomycin or vancomycin might be the champion you need. And remember, every dollar saved on a drug can go toward a warm cup of tea for the patient’s recovery journey! 🎉
watch the blood work with linezolid its a must
Linezolid is a double‑edged sword its power is real but the blood fad can drain you
Pick linezolid for lungs avoid vancomycin if kidneys hurt