Minocycline vs Alternatives: Antibiotic Comparison Tool
| Attribute | Minocycline (Minocin) |
Doxycycline | Tetracycline | Amoxicillin | Azithromycin | Clindamycin |
|---|---|---|---|---|---|---|
| Class | Tetracycline | Tetracycline | Tetracycline | Penicillin | Macrolide | Lincosamide |
| Typical Uses | Acne, rosacea, rheumatoid arthritis, skin infections | Acne, Lyme disease, malaria prophylaxis | Broad-spectrum bacterial infections | Sinusitis, otitis media, bronchitis | Community-acquired pneumonia, chlamydia | MRSA, anaerobic skin/soft-tissue infections |
| Dosage Range (adults) | 100 mg once daily | 100 mg twice daily | 250-500 mg every 6 h | 500 mg three times daily | 500 mg day 1, then 250 mg daily for 4 days | 300 mg four times daily |
| Common Side Effects | Vertigo, skin discoloration, lupus-like syndrome | Photosensitivity, upset stomach | Nausea, gastro-esophageal irritation | Allergic rash, diarrhea | GI upset, QT prolongation | Diarrhea, C. difficile infection |
| Pregnancy Category (US) | D (risk present) | D | D | B (generally safe) | Category B | C (risk cannot be ruled out) |
| Average Monthly Cost (US, retail) | $45-$70 (generic) | $30-$55 | $25-$40 | $15-$25 | $20-$35 | $35-$60 |
When you’re prescribed an oral antibiotic for acne, skin infections, or even rheumatoid arthritis, you quickly discover there are a few names that keep popping up. Minocycline is one of them, marketed as Minocin, but how does it really stack up against the other options on the shelf? This guide walks you through the science, the side‑effects, and the cost factors so you can decide whether Minocycline is the right fit or if another drug makes more sense.
Key Takeaways
- Minocycline is a broad‑spectrum tetracycline antibiotic with strong activity against acne‑causing bacteria and certain respiratory pathogens.
- Common alternatives-doxycycline, tetracycline, amoxicillin, azithromycin, and clindamycin-vary in spectrum, side‑effect profile, and pregnancy safety.
- Minocycline often costs more but offers once‑daily dosing and can treat inflammatory skin conditions better than many peers.
- Patients with liver disease, pregnancy, or a history of drug‑induced lupus should consider non‑tetracycline options.
- Understanding dosage range, typical uses, and insurance coverage helps avoid surprise out‑of‑pocket expenses.
How Minocycline Works
Minocycline is a synthetic tetracycline antibiotic that inhibits bacterial protein synthesis by binding to the 30S ribosomal subunit. This binding blocks the addition of new amino acids to the growing peptide chain, effectively stopping bacterial growth. Because it’s lipophilic, Minocycline penetrates skin and joint tissues well, making it a popular choice for treating moderate to severe acne and certain rheumatologic conditions. The drug is usually taken once a day, which improves adherence compared with older tetracyclines that require multiple doses.
Popular Alternatives Overview
Below are the most frequently prescribed antibiotics that patients compare with Minocycline. Each entry includes a brief definition with microdata markup on first appearance.
- Doxycycline is another tetracycline derivative, often used for Lyme disease, malaria prophylaxis, and acne. It shares the same mechanism as Minocycline but has a slightly shorter half‑life, leading to twice‑daily dosing for many indications.
- Tetracycline is the prototype of the class. While effective against a broad range of bacteria, it requires dosing every six hours and has a higher incidence of gastrointestinal upset.
- Amoxicillin belongs to the penicillin family. It targets cell‑wall synthesis and is widely used for ear, sinus, and throat infections. It’s safe in pregnancy but ineffective against many tetracycline‑resistant organisms.
- Azithromycin is a macrolide that inhibits bacterial protein synthesis at the 50S ribosomal subunit. Its long half‑life allows a three‑day course for many respiratory infections, but it can cause QT‑prolongation in susceptible patients.
- Clindamycin is a lincosamide antibiotic that also blocks the 50S ribosomal subunit. It’s effective against anaerobic skin infections and MRSA, though it carries a higher risk of Clostridioides difficile colitis.
Side‑Effect Snapshot
All antibiotics have trade‑offs. Minocycline’s unique side‑effects include a potential for drug‑induced lupus‑like syndrome and permanent pigmentation of teeth or skin, especially with long‑term use. Doxycycline can cause photosensitivity, while tetracycline often leads to nausea. Amoxicillin, being a β‑lactam, may trigger allergic reactions ranging from rash to anaphylaxis. Azithromycin is generally well‑tolerated but may provoke heart rhythm changes. Clindamycin’s biggest red flag is its association with severe diarrhea due to C. difficile.

Comparison Table
| Attribute | Minocycline (Minocin) | Doxycycline | Tetracycline | Amoxicillin | Azithromycin | Clindamycin |
|---|---|---|---|---|---|---|
| Class | Tetracycline | Tetracycline | Tetracycline | Penicillin | Macrolide | Lincosamide |
| Typical Uses | Acne, rosacea, rheumatoid arthritis, skin infections | Acne, Lyme disease, malaria prophylaxis | Broad‑spectrum bacterial infections | Sinusitis, otitis media, bronchitis | Community‑acquired pneumonia, chlamydia | MRSA, anaerobic skin/soft‑tissue infections |
| Dosage Range (adults) | 100mg once daily | 100mg twice daily | 250‑500mg every 6h | 500mg three times daily | 500mg day1, then 250mg daily for 4days | 300mg four times daily |
| Common Side‑Effects | Vertigo, skin discoloration, lupus‑like syndrome | Photosensitivity, upset stomach | Nausea, gastro‑esophageal irritation | Allergic rash, diarrhea | GI upset, QT prolongation | Diarrhea, C. difficile infection |
| Pregnancy Category (US) | D (risk present) | D | D | B (generally safe) | Category B | C (risk cannot be ruled out) |
| Average Monthly Cost (US, retail) | $45‑$70 (generic) | $30‑$55 | $25‑$40 | $15‑$25 | $20‑$35 | $35‑$60 |
When Minocycline Is the Better Choice
If you need a drug that gets deep into the skin and joints, Minocycline’s lipophilic nature gives it an edge over doxycycline and tetracycline. Its once‑daily schedule also improves compliance, especially for teenagers dealing with acne. For patients who have tried other tetracyclines without success, the slightly higher potency of Minocycline can make the difference. Moreover, for off‑label use in rheumatoid arthritis, Minocycline’s anti‑inflammatory properties are valuable.
Scenarios Where Alternatives Shine
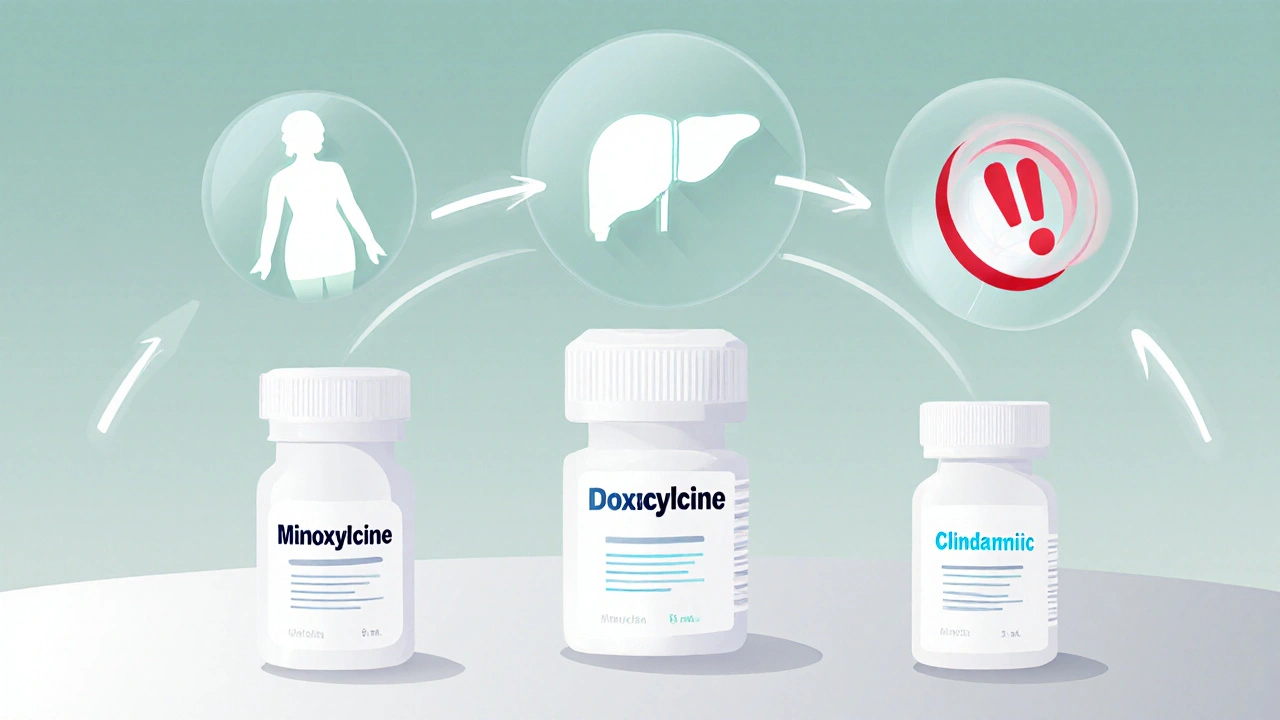
Not every case calls for Minocycline. If a patient is pregnant, isotretinoin‑compatible antibiotics like amoxicillin or azithromycin become safer bets. Those with a history of liver dysfunction should avoid Minocycline because it’s metabolized hepatically; doxycycline may be less taxing, but still requires monitoring.
When the infection is caused by beta‑lactamase‑producing organisms, amoxicillin combined with clavulanate outperforms any tetracycline. For rapid, short‑course therapy-think uncomplicated pneumonia-azithromycin’s three‑day regimen beats a ten‑day Minocycline course in convenience. Finally, if MRSA is on the differential, clindamycin offers better coverage than Minocycline, assuming the patient can tolerate the higher C. difficile risk.
Safety, Interactions, and Insurance Tips
All antibiotics can interact with other meds. Minocycline may increase the effect of anticoagulants like warfarin, and it can reduce the efficacy of oral contraceptives-a crucial point for women of child‑bearing age. Doxycycline shares the contraceptive interaction but also binds calcium, so avoid taking it with dairy products.
Insurance plans often place Minocycline on a higher tier, leading to larger copays. Checking the formulary ahead of time can prevent surprise bills. Generic versions are typically cheaper, but not every pharmacy stocks them. In such cases, broaching the alternative options with your prescriber can yield a more affordable regimen without sacrificing efficacy.
Bottom Line Decision Flow
- Identify the infection type (acne, respiratory, skin, MRSA, etc.).
- Check patient‑specific factors: pregnancy, liver/kidney health, drug allergies.
- Match the infection to the most effective class (tetracycline, penicillin, macrolide, lincosamide).
- Consider dosing convenience and cost.
- Discuss with your clinician and confirm insurance coverage.
Following this flow helps you land on the right antibiotic without unnecessary trial‑and‑error.
Frequently Asked Questions
Can I take Minocycline for acne if I’m pregnant?
No. Minocycline is classified as Pregnancy Category D, which means there is evidence of risk to the fetus. Safer alternatives like amoxicillin or azithromycin should be considered.
Why does Minocycline sometimes cause a bluish skin tint?
The drug can deposit in melanin‑rich tissues, especially with long‑term therapy. This pigmentation is usually permanent but harmless. If the appearance bothers you, discuss switching to doxycycline, which has a lower risk.
Is Minocycline effective against MRSA?
Some MRSA strains are susceptible, but clindamycin or trimethoprim‑sulfamethoxazole are typically preferred first‑line options because they have more reliable activity.
Can I take Minocycline with my birth control pills?
Minocycline can reduce the effectiveness of hormonal contraceptives. Use a backup method (e.g., condoms) while on the antibiotic and for at least a week after finishing the course.
Which antibiotic is cheapest for a 30‑day acne regimen?
Generally, generic tetracycline or doxycycline are the most affordable, ranging from $25‑$55 per month. Minocycline tends to be pricier, especially if you need the brand‑name version.



10 Comments
The reckless over‑use of broad‑spectrum antibiotics threatens our nation's health security.
Minocycline, while effective, should be reserved for cases where alternatives fail.
Prescribing it indiscriminately encourages resistant bacteria.
Our clinicians must adhere to strict stewardship guidelines.
Patients also bear the financial burden of unnecessary therapy.
By limiting use, we protect both public health and the economy.
While Minocycline offers convenient once‑daily dosing, the decision matrix must consider infection type, patient comorbidities, and cost.
For acne, doxycycline provides comparable efficacy with a lower price point.
In respiratory infections, azithromycin’s short course can improve adherence.
Nevertheless, for rheumatoid arthritis, Minocycline’s anti‑inflammatory properties remain unique.
Thus, clinicians should match the drug to the clinical scenario rather than default to familiarity.
It is encouraging to see tools that let patients compare antibiotics side‑by‑side.
Understanding the side‑effect profile empowers individuals to have informed discussions with their providers.
For those worried about photosensitivity, doxycycline’s warning is a useful reminder to use sunscreen.
Similarly, the pigmentation risk of Minocycline highlights the importance of monitoring during long‑term therapy.
Overall, such transparency fosters shared decision‑making.
Antonio, you made a solid point about tailoring therapy.
Adding that insurance formularies often place Minocycline on a higher tier can further guide the choice.
When a patient’s copay becomes prohibitive, discussing generic tetracycline or doxycycline may avoid financial strain.
Always verify formulary status before finalizing the prescription.
Cost is a big factor for many patients.
Indeed, the monthly price range shown in the table illustrates why affordability matters.
For a typical acne regimen, doxycycline can be as low as $30, whereas Minocycline may exceed $60.
This difference can affect adherence, especially for uninsured individuals.
Minocycline’s pharmacokinetic profile distinguishes it from other tetracyclines in several clinically relevant ways.
First, its high lipophilicity allows deeper penetration into skin and synovial fluid, which is advantageous for treating acne and rheumatoid arthritis.
Second, the once‑daily dosing schedule reduces pill burden, an important consideration for adolescents who struggle with compliance.
Third, the drug’s half‑life supports steady plasma concentrations, minimizing peak‑related adverse effects.
However, these benefits come with unique risks, such as drug‑induced lupus‑like syndrome, which can manifest as joint pain, fever, and serologic abnormalities.
Patients should be educated to report any such systemic symptoms promptly.
Another notable side effect is permanent hyperpigmentation, especially in areas of inflammation, which may be cosmetically distressing.
Contraindications include pregnancy (Category D) and significant hepatic impairment, given the drug’s metabolism in the liver.
For individuals with a prior history of liver disease, doxycycline may be a safer alternative, though it still requires monitoring.
Cost considerations also play a pivotal role; the generic form of Minocycline often costs between $45 and $70 per month, which can be a barrier for some patients.
Insurance plans frequently tier Minocycline higher than doxycycline or tetracycline, leading to higher out‑of‑pocket expenses.
When insurance coverage is limited, clinicians might prioritize a less expensive tetracycline, accepting the need for more frequent dosing.
In the context of MRSA infections, clindamycin generally offers superior coverage, but Minocycline retains activity against certain strains and can be used when clindamycin resistance is documented.
The drug’s interaction profile includes potentiation of anticoagulants like warfarin, necessitating close INR monitoring.
Finally, Minocycline can diminish the efficacy of hormonal contraceptives, so additional birth control methods should be advised for women of reproductive age.
Overall, while Minocillin provides distinct pharmacologic advantages, its use should be judicious, balancing efficacy, safety, and economic factors.
While the list of concerns is comprehensive, it overlooks the real‑world scenario where many patients tolerate Minocycline without any pigment changes.
Moreover, the convenience of a single daily dose often outweighs modest cost differences for those with stable insurance.
Thus, discarding Minocycline solely on potential side effects may be overly cautious.
Seeing how each antibiotic shines in different niches really helps demystify treatment choices.
Indeed, matching the drug to the infection’s niche optimizes outcomes and minimizes unnecessary exposure.