Sleep Apnea & Heart Rhythm Risk Calculator
How Sleep Apnea Affects Your Heart Rhythm
Sleep apnea is linked to a higher risk of heart rhythm disorders like atrial fibrillation and ventricular ectopy. This tool assesses your personal risk based on key factors. Your results will show your risk level and explain how sleep apnea impacts heart rhythm.
Risk Assessment
Answer the following questions about your health and lifestyle to calculate your risk level.
Your Risk Assessment
What your score means:
Recommendations
When researchers look at sleep apnea is a repetitive blockage of the airway during sleep that leads to brief pauses in breathing, they often find a surprising link to the heart’s rhythm. If you’ve ever woken up feeling exhausted, or noticed a racing heart after a night of snoring, you might be wondering whether the two are connected. This article unpacks the science, the numbers, and the practical steps you can take to protect your heart.
What Exactly Is Sleep Apnea?
Sleep apnea falls into three main categories:
- Obstructive Sleep Apnea (OSA) is the most common form, caused by soft tissue collapsing and blocking the airway.
- Central Sleep Apnea (CSA) occurs when the brain fails to send proper signals to the breathing muscles.
- Complex (mixed) Sleep Apnea combines features of both OSA and CSA.
Typical symptoms include loud snoring, witnessed pauses, morning headaches, and daytime fatigue. The severity is measured by the Apnea‑Hypopnea Index (AHI), which counts the number of breathing interruptions per hour of sleep.
Understanding Heart Rhythm Disorders
Heart rhythm disorders, or arrhythmias, are abnormalities in the electrical impulses that coordinate heartbeats. The most common types are:
- Atrial Fibrillation (AF) - rapid, irregular beating of the atria.
- Ventricular Tachycardia (VT) - fast beats originating from the ventricles, potentially life‑threatening.
- Premature atrial or ventricular contractions, which are extra beats that feel like a “flutter” or “skip.”
Arrhythmias can lead to stroke, heart failure, or sudden cardiac death, especially when they go untreated.
How Sleep Apnea Messes With Your Heart
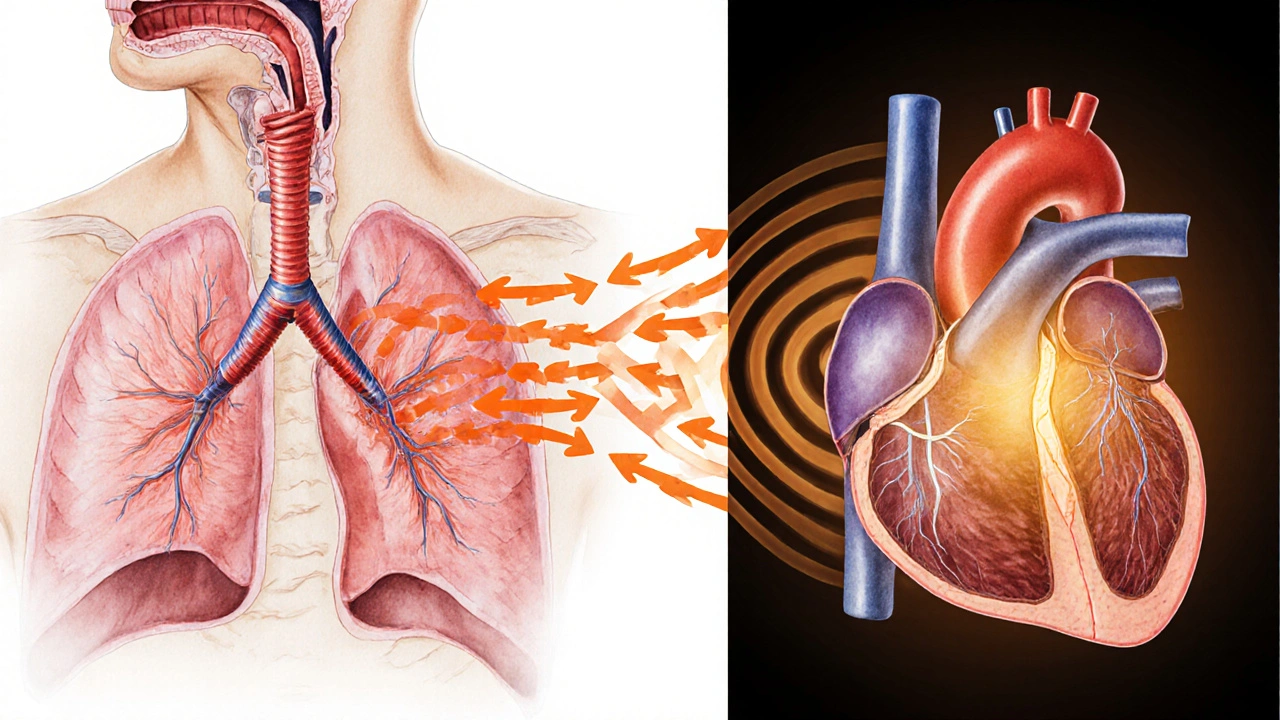
Three physiological mechanisms explain the link:
- Oxygen desaturation: Each apnea episode drops blood oxygen levels, triggering oxidative stress and inflammation.
- Sympathetic nervous system activation: The body reacts to low oxygen by releasing adrenaline, raising heart rate and blood pressure.
- Intrathoracic pressure swings: The effort to breathe against a blocked airway creates negative pressure, stretching the heart chambers and altering electrical conduction.
Over time, these stressors remodel heart tissue, making it more prone to irregular electrical signals.
What the Research Says
Large cohort studies provide solid numbers. A 2023 analysis of 15,000 adults found that people with moderate‑to‑severe OSA (AHI≥15) had a 2.5‑fold higher incidence of new‑onset AF over five years compared to those without OSA. Another investigation using implantable cardiac monitors reported that nocturnal apnea episodes increased the odds of ventricular ectopy by 1.8×. The Takeaway: the relationship isn’t just anecdotal-it’s statistically significant.
Who Is Most at Risk?
Risk factors stack up like a checklist:
- Obesity (BMI>30) - excess neck fat narrows the airway.
- Male sex - men develop OSA 2‑3 times more often than women.
- Age over 50 - muscle tone declines, making collapse easier.
- Hypertension or existing cardiovascular disease - already sensitized heart tissue.
- Family history of sleep‑disordered breathing.
If you tick several boxes, you should discuss screening with your doctor.
Getting a Diagnosis
The gold‑standard test is polysomnography (sleep study), which records breathing effort, oxygen saturation, brain waves, and heart rhythm overnight. For people who can’t spend a night in a lab, home‑sleep testing devices capture AHI and oxygen desaturation index (ODI) but may miss subtle arrhythmia signals.
Because the heart is involved, many clinicians add a resting ECG or, if symptoms suggest it, a 24‑hour Holter monitor to spot intermittent arrhythmias.
Managing Both Conditions
Treating sleep apnea often improves heart rhythm outcomes. The most evidence‑based approach is continuous positive airway pressure (CPAP) therapy, which keeps the airway open by delivering a steady stream of air.
Key benefits observed in trials:
- Reduction of AF recurrence after catheter ablation by ~30%.
- Lower nighttime blood pressure spikes, decreasing strain on the heart.
- Decreased sympathetic activity, measured by heart‑rate variability.
If CPAP isn’t tolerated, alternatives include dental mandibular advancement devices, positional therapy, and in severe cases, upper‑airway surgery.
On the cardiac side, doctors may prescribe anti‑arrhythmic drugs, anticoagulants (for AF), or recommend lifestyle changes such as weight loss, reduced alcohol intake, and regular aerobic exercise.

Practical Checklist for Patients
- Ask your physician for a sleep study if you snore loudly, wake gasping, or feel unusually fatigued.
- Track your blood pressure and heart rate at home; note any night‑time spikes.
- If diagnosed with OSA, commit to using CPAP every night - even naps.
- Schedule regular cardiac follow‑ups, especially if you have hypertension or a history of arrhythmia.
- Adopt heart‑healthy habits: lose excess weight, limit caffeine/alcohol, and aim for 150minutes of moderate exercise per week.
Comparison of Arrhythmia Risk With and Without Sleep Apnea
| Study | Population | Arrhythmia Type | Prevalence in OSA (%) | Prevalence in Controls (%) |
|---|---|---|---|---|
| 2023 Cohort, USA | 15,000 adults | Atrial Fibrillation | 12.4 | 5.0 |
| 2022 Implantable Monitor, Europe | 2,500 patients with cardiac devices | Ventricular Ectopy | 9.1 | 4.7 |
| 2021 Sleep‑Heart Study, Japan | 8,000 community members | Premature Atrial Beats | 15.3 | 7.8 |
Key Takeaways
- The link between sleep apnea heart rhythm disorders is backed by robust clinical data.
- Untreated OSA dramatically raises the risk of atrial fibrillation, ventricular ectopy, and sudden cardiac events.
- CPAP therapy not only improves sleep quality but also reduces arrhythmia recurrence.
- Early screening-especially for overweight, middle‑aged men-can catch both conditions before serious damage occurs.
- Combining lifestyle changes with appropriate medical treatment offers the best protection for heart and sleep health.
Frequently Asked Questions
Can sleep apnea cause a heart attack?
Yes. Repeated oxygen drops and surges in blood pressure strain the coronary arteries, increasing the likelihood of plaque rupture and myocardial infarction, especially in people with existing atherosclerosis.
If I’ve been diagnosed with atrial fibrillation, should I be tested for sleep apnea?
Absolutely. Guidelines from major cardiology societies recommend polysomnography for all newly diagnosed AF patients because treating underlying OSA improves rhythm‑control success.
Does CPAP completely eliminate the risk of arrhythmias?
CPAP significantly reduces risk but does not guarantee zero recurrence. Weight loss, blood‑pressure control, and, when needed, anti‑arrhythmic medication remain essential components of care.
Are home sleep tests reliable for detecting the heart‑rhythm impact?
Home tests accurately measure AHI and oxygen desaturation, but they usually don’t record detailed ECG data. If you have cardiovascular symptoms, a full in‑lab study is preferable.
What lifestyle changes help both sleep apnea and arrhythmia risk?
Losing excess weight, limiting alcohol (especially before bedtime), quitting smoking, and engaging in regular moderate‑intensity aerobic activity improve airway patency and lower sympathetic tone, benefiting both conditions.




13 Comments
Screening for sleep apnea early can spare you from future heart rhythm complications.
Hey, great article! If you’re feeling the fatigue after a night of snoring, consider getting a sleep study-early detection can make a huge difference. CPAP isn’t always fun, but sticking with it can cut down arrhythmia risk dramatically. Pair that with a bit of weight loss and less late‑night booze, and you’ll be giving your heart a solid break. Keep pushing forward, you’ve got this!
Listen, I’m not one to sugar‑coat shit, but you’re basically ignoring a ticking time bomb if you skip the test. The research isn’t some flimsy anecdote; it’s a massive cohort that shows OSA cranks up AF risk by 2.5 times-yeah, that’s real. And don’t tell me you’re too busy for a night in a lab; your heart won’t wait for your schedule. The oxygen dips, the adrenaline spikes, the pressure swings-they all mash your heart’s wiring. So get the study, get the treatment, get your life back. Stop dithering and act.
It’s easy to feel overwhelmed by the medical jargon, but taking one step at a time-like talking to your doctor-can really ease the stress.
Wow!!! This post really breaks down the crazy link between sleep apnea and heart rhythm problems!!! If you’re over 30 and snore like a freight train, you’re basically waving a red flag for AF!!! Don’t wait-talk to a specialist, get a sleep study, and consider CPAP!!! Your heart will thank you!!!
For anyone interested in the practical side, the gold‑standard polysomnography captures both breathing disruptions and ECG data, which helps correlate apnea events with arrhythmia episodes. Home sleep monitors are convenient but may miss subtle ECG changes, so a full night in a sleep lab remains the most comprehensive option.
Key take‑away: early screening, CPAP adherence, weight management, and regular cardiac check‑ups are the pillars of protecting both sleep and heart health.
Sleep apnea isn’t just a noisy night-it’s a silent architect of cardiac chaos. When the airway collapses, oxygen levels plunge, and the body screams with adrenaline. That surge of sympathetic activity jolts the heart’s rhythm like a badly tuned drum. Repeated drops in oxygen create oxidative stress that remodels heart tissue. Over time, the atria become a breeding ground for erratic electrical signals. Studies show a 2.5‑fold increase in atrial fibrillation for moderate‑to‑severe OSA patients. Even ventricular ectopy rates climb by nearly double in the same cohort. The good news? CPAP therapy can shave off up to thirty percent of arrhythmia recurrence. Consistency is key-skipping nights on the machine erodes those benefits fast. Weight loss not only eases airway obstruction but also reduces the heart’s workload. Limiting alcohol before bedtime cuts down on throat muscle relaxation, improving airflow. Regular aerobic exercise boosts cardiovascular resilience and stabilizes heart rhythm. If you’re over fifty, male, or carry extra weight, the risk stack grows taller. Don’t wait for a scary episode; proactive screening can catch the problem early. In short, treat the sleep apnea and you’re treating the heart-two birds, one stone! 😎
Indeed, the heart and the night are entwined in a dance of shadows; neglecting one partner inevitably throws the other off‑beat, and the resulting discord can echo through a lifetime.
Take the first step today-your future self will thank you for the breath of life you give your heart.
The night whispers its secrets to those who listen, and in the hush of a night punctuated by snoring, the heart’s rhythm may falter like a candle in a storm; yet, armed with knowledge and the resolve to seek help, we can turn that trembling flame into a steadfast beacon of health.
Sleep well, heart happy 😊
For anyone considering CPAP, make sure to get a proper mask fit; leaks can reduce effectiveness and cause skin irritation, which many users overlook.