Desmopressin Dosage Calculator
Desmopressin Dosage Calculator
This tool helps determine appropriate desmopressin dosage based on urine output and patient factors for Central Diabetes Insipidus.
Input Your Data
Recommended Dosage
Enter your urine output to see recommendations
Central Diabetes Insipidus is a rare condition where the brain stops making enough antidiuretic hormone, leading to excessive thirst and urination. Understanding how the body's defense network ties into this disorder helps patients and clinicians spot hidden causes and choose smarter treatments.
What Exactly Is Central Diabetes Insipidus?
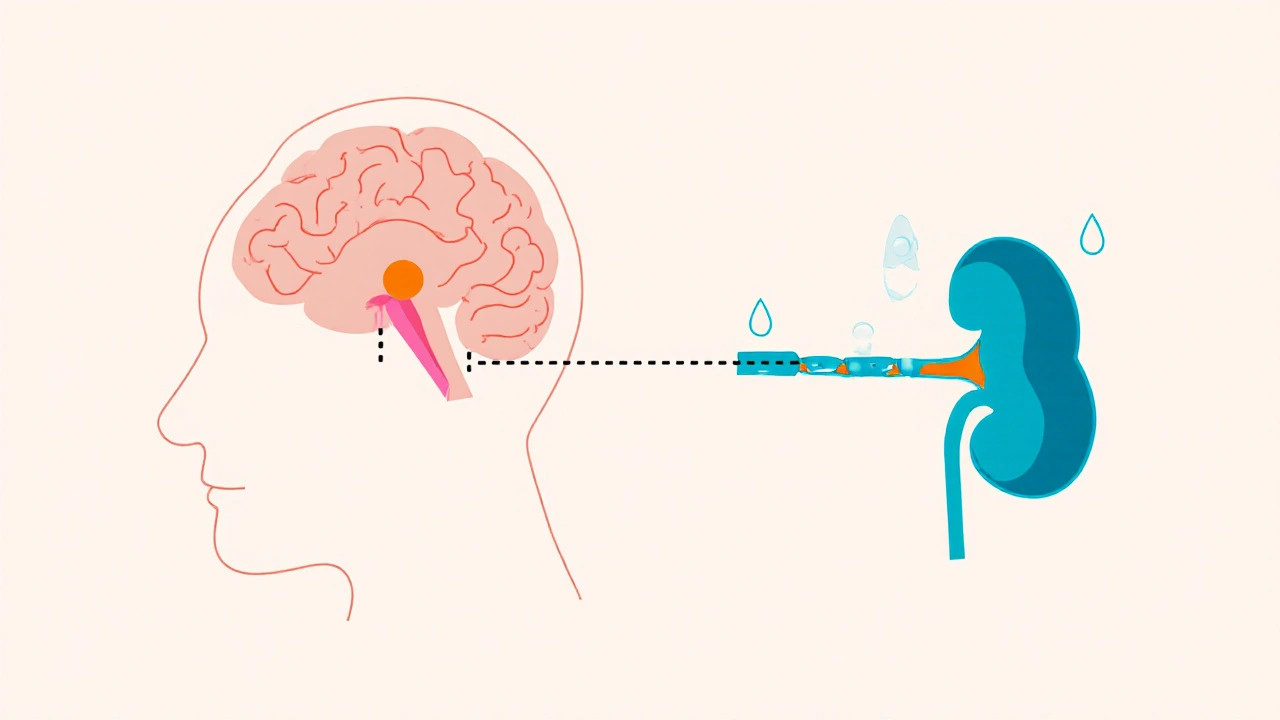
When the Central Diabetes Insipidus a disorder caused by insufficient production of vasopressin in the brain occurs, the kidneys cannot re‑absorb water properly. The result is a flood of dilute urine and a constant need to drink. Unlike the more common nephrogenic form, CDI originates in the brain, specifically the Pituitary Gland a pea‑sized organ that releases hormones into the bloodstream and the Hypothalamus the brain region that controls hormone release.
Key symptoms include:
- Polyuria (large volumes of urine)
- Polydipsia (unquenchable thirst)
- Nocturia (waking up to pee)
- Potential dehydration if fluid intake cannot keep up
How the Immune System Can Trigger CDI
The Immune System the body's network of cells and molecules that defend against infection sometimes turns against itself, a phenomenon called autoimmunity. Certain Autoimmune Diseases conditions where the immune system attacks healthy tissue are known to affect the hypothalamic‑pituitary axis. For example, lymphocytic hypophysitis inflames the pituitary, reducing its ability to release vasopressin.
Inflammatory Cytokines protein messengers that coordinate immune responses such as interleukin‑6 (IL‑6) and tumor necrosis factor‑α (TNF‑α) can disrupt the delicate balance of hormone secretion. In some patients, a viral infection sparks a cascade of cytokines that temporarily shut down vasopressin production, creating a reversible form of CDI.
Clinical Clues That Point to an Immune Link
When CDI shows up alongside signs of systemic inflammation, doctors start suspecting an immune trigger. Look for:
- Unexplained fever or malaise
- Elevated inflammatory markers (CRP, ESR) on blood tests
- Concurrent autoimmune symptoms like joint pain, skin rashes, or thyroid dysfunction
- Imaging that reveals pituitary enlargement or stalk thickening
These patterns often appear in patients with lupus, sarcoidosis, or granulomatous diseases that can invade the hypothalamic‑pituitary region.
Diagnosing an Immune‑Related CDI
Standard CDI work‑up includes water deprivation tests and measurement of serum and urine osmolality. To uncover an immune cause, add these steps:
- Order a full panel of Autoantibody blood proteins that target the body's own tissues (e.g., anti‑pituitary, anti‑hypothalamic antibodies).
- Check inflammatory markers: C‑reactive protein (CRP), erythrocyte sedimentation rate (ESR), and cytokine profiles.
- Take a high‑resolution MRI magnetic resonance imaging of the brain focusing on the sellar region to spot pituitary inflammation or mass lesions.
- Consider a lumbar puncture if central nervous system infection is suspected; look for pleocytosis and viral PCR.
Combining hormonal data with immune markers helps differentiate primary autoimmune CDI from secondary causes like tumors or head trauma.
Treatment Strategies That Address Both Hormone Deficit and Inflammation
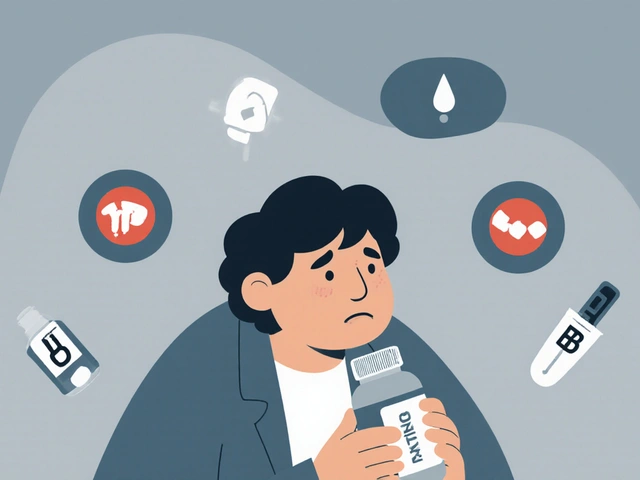
The backbone of CDI therapy is Desmopressin a synthetic analogue of vasopressin used to reduce urine output. However, when an immune process is driving the problem, additional steps are required:
- Immunosuppression: Low‑dose prednisone or other corticosteroids can dampen pituitary inflammation quickly. In chronic cases, steroid‑sparing agents like azathioprine or mycophenolate may be added.
- Targeted biologics: For patients with high IL‑6 levels, tocilizumab (an IL‑6 receptor blocker) has shown promise in restoring normal vasopressin release.
- Monitor Water Balance the equilibrium between fluid intake and loss closely. Adjust desmopressin dose as inflammation subsides; overtreatment can cause hyponatremia.
- Regular imaging: Repeat MRI every 6-12 months to ensure the pituitary returns to normal size.
Collaboration between endocrinologists and immunologists speeds up diagnosis and tailors therapy to the individual's immune profile.
Living With Immune‑Linked CDI: Practical Tips
Even with medication, day‑to‑day management matters:
- Carry a medical alert card that lists CDI, current immunosuppressants, and the desmopressin dose.
- Track fluid intake and urine output using a simple notebook or mobile app.
- Avoid rapid changes in temperature; extreme heat can increase fluid loss.
- Stay up to date on vaccinations, especially for flu and pneumococcus, to reduce infection‑driven cytokine spikes.
- Schedule quarterly blood work to catch rising CRP or autoantibody titres before symptoms flare.
These habits empower patients to spot a hidden immune flare early, preventing unnecessary hospital visits.
Key Takeaways
- Central Diabetes Insipidus stems from insufficient vasopressin production in the pituitary‑hypothalamic axis.
- Autoimmune inflammation, cytokine storms, and infections can all transiently or permanently disrupt vasopressin release.
- Combining hormonal testing with autoantibody panels, cytokine levels, and pituitary MRI improves diagnostic accuracy.
- Treatment blends desmopressin with appropriate immunosuppressive or biologic therapy.
- Active self‑monitoring and coordinated specialist care are essential for long‑term stability.
| Marker | Typical Range | Relevance to CDI |
|---|---|---|
| CRP | <5 mg/L | Elevated levels suggest active inflammation that may impair vasopressin release. |
| IL‑6 | 0-7 pg/mL | High IL‑6 correlates with cytokine‑mediated pituitary dysfunction. |
| Anti‑Pituitary Antibody (APA) | Negative | Positive APA points toward autoimmune hypophysitis as a cause. |
| ANA (antinuclear antibody) | Negative | Often positive in systemic lupus, which can involve the hypothalamus. |
Frequently Asked Questions
Can an infection cause sudden onset of CDI?
Yes. Certain viral infections trigger a cytokine surge that temporarily shuts down vasopressin production, leading to acute polyuria and polydipsia. The condition often resolves once the infection clears, but monitoring is essential.
Is lymphocytic hypophysitis the same as CDI?
Lymphocytic hypophysitis is an autoimmune inflammation of the pituitary. When it damages the cells that secrete vasopressin, patients develop secondary CDI. Treating the inflammation often improves hormone levels.
How does desmopressin differ from natural vasopressin?
Desmopressin is a synthetic analogue that lasts longer and has less effect on blood pressure. It specifically targets kidney water channels, making it ideal for CDI without causing the vasoconstriction seen with natural vasopressin.
Should I get a repeat MRI after starting immunosuppression?
A follow‑up MRI at 6‑12 months helps confirm that pituitary inflammation is receding. Persistent enlargement may signal an alternate diagnosis that needs further work‑up.
Can lifestyle changes reduce the immune impact on CDI?
While diet alone won’t cure CDI, maintaining a balanced anti‑inflammatory diet, regular sleep, and stress management can lower baseline cytokine levels, making flare‑ups less likely.


9 Comments
Wow, another hormone puzzle-just what your weekend needed! But hey, you’ve got desmopressin, a bit of steroid, and a killer tracking app, so you’re basically a superhero in a lab coat. Keep that water bottle handy, and remember: every pee is a reminder you’re still alive. If the cytokine storm tries to crash the party, just give it a firm “nope” and let the endocrinologist handle the fireworks. Stay thirsty, stay victorious! 😏
My dear fellow aficionados of endocrinology, the intricate dance between vasopressin and cytokines is nothing short of a symphonic masterpiece. One must appreciate the elegance of juxtaposing hormonal replacement with judicious immunomodulation. It is, after all, the epitome of personalized medicine-where art meets science in the most delightful of embraces. Cheers to the clinicians who wield both the scalpel and the syringe with such finesse.
Ah, the ever‑mysterious liaison of the pituitary and the immune battalion, a topic that beckons the soul to wander the corridors of ancient lore and modern lab reports alike. 🌌
One could argue that vasopressin itself is a silent philosopher, whispering water‑balance truths to the kidneys while the cytokine chorus sings of inflammation.
When IL‑6 creeps onto the stage, it does so with the subtlety of a Shakespearean villain, nudging the hypothalamus into a pause that feels almost poetic.
Yet, let us not romanticize the suffering; the patient’s nocturnal pilgrimages to the bathroom are as real as any epic quest.
In the grand theater of autoimmunity, lymphocytic hypophysitis plays the role of the tragic hero, its autoimmune thrust both noble and cruel.
The clinician, armed with desmopressin, becomes the modern alchemist, transmuting synthetic peptide into reclaimed homeostasis.
But the alchemy does not end there; steroids, azathioprine, tocilizumab-each is a rune etched upon the patient’s chart, promising order amidst chaos.
Consider the fluid‑tracking app a digital oracle, mapping the ebb and flow of existence with the precision of a monk copying sacred texts.
And what of the MRI? Those high‑resolution images are like Da Vinci’s sketches, revealing the hidden architecture of the sellar realm.
We must also acknowledge the humility required to listen to the patient’s own narrative - the sweaty palms, the relentless thirst, the fear of hyponatremia.
Every lab value is a stanza in a poem that only the interdisciplinary team can fully read.
Thus, the interplay of immunity and CDI is not merely pathology; it is a micro‑cosm of the body’s eternal negotiation between destruction and repair.
Let us, therefore, celebrate the paradox: that a virus‑induced cytokine storm can both betray and heal, that an autoimmune attack can be tamed with a carefully dosed steroid.
In the end, the story is one of resilience, a reminder that the human organism is both scholar and student in its own right.
Stay curious, stay compassionate, and never underestimate the power of a well‑timed emoji. 😇
Hey everyone! 🌍 Just wanted to shout out that these immune‑linked CDI cases remind us how interconnected our bodies really are. If you notice any extra symptoms like joint aches or a rash, bring them up with your doctor – it could be a clue that the immune system is involved. And remember, sharing knowledge helps us all stay healthier, so keep those experiences coming!
Alright team, let’s paint this picture in full color! 🎨 Central Diabetes Insipidus might sound like a dry topic, but when the immune system tosses in its own palette of cytokines, the whole canvas bursts with nuance. Think of desmopressin as the bright splash of blue that steadies the water‑balance, while steroids and biologics add the bold reds and golds of inflammation control. Keep that diary open, track every sip and every pee – it’s the brushstroke that tells the real story. And don’t forget: a glittering MRI now and then is the sparkle that confirms we’re on the right track. Stay vibrant, stay vigilant, and let’s turn this clinical challenge into a masterpiece! 🌟
Here’s the quick rundown you need – start with a water deprivation test to confirm the polyuria, then check serum and urine osmolality. Next, grab a full auto‑antibody panel (APA, ANA, etc.) and a high‑resolution pituitary MRI. If you see elevated CRP or IL‑6, add low‑dose prednisone and watch the response. For refractory cases, consider tocilizumab if IL‑6 is sky‑high. Adjust desmopressin dose based on the fluid balance chart and re‑check electrolytes weekly to avoid hyponatremia. Keep the endocrine‑immunology team in the loop and schedule follow‑up imaging at 6‑month intervals.
Sure, that “standard” protocol sounds neat on paper, but let’s not pretend the pharma‑driven guidelines aren’t steering us into a maze of unnecessary meds. Often the immune trigger is fleeting, and piling on steroids only masks the real issue while inviting a host of side‑effects. Maybe the body’s cytokine surge is just a signal, not a disease, and we should be looking at lifestyle, gut health, and environmental toxins before throwing a cocktail of immunosuppressants at the patient.
Oh, look, another “enthusiastic” post about balancing hormones with fancy drugs. As if patients haven’t already been walking on a tightrope of side‑effects. Adding “low‑dose prednisone” to the list feels like adding glitter to a dumpster fire – it looks shiny but does nothing to fix the underlying mess. Honestly, the whole approach just drags people deeper into a pharmacy dependency while the real conversation about holistic care gets left in the dust.
Sounds like a typical day for a hormone‑hunted adventurer.