Why skin colour can change when fungi move in
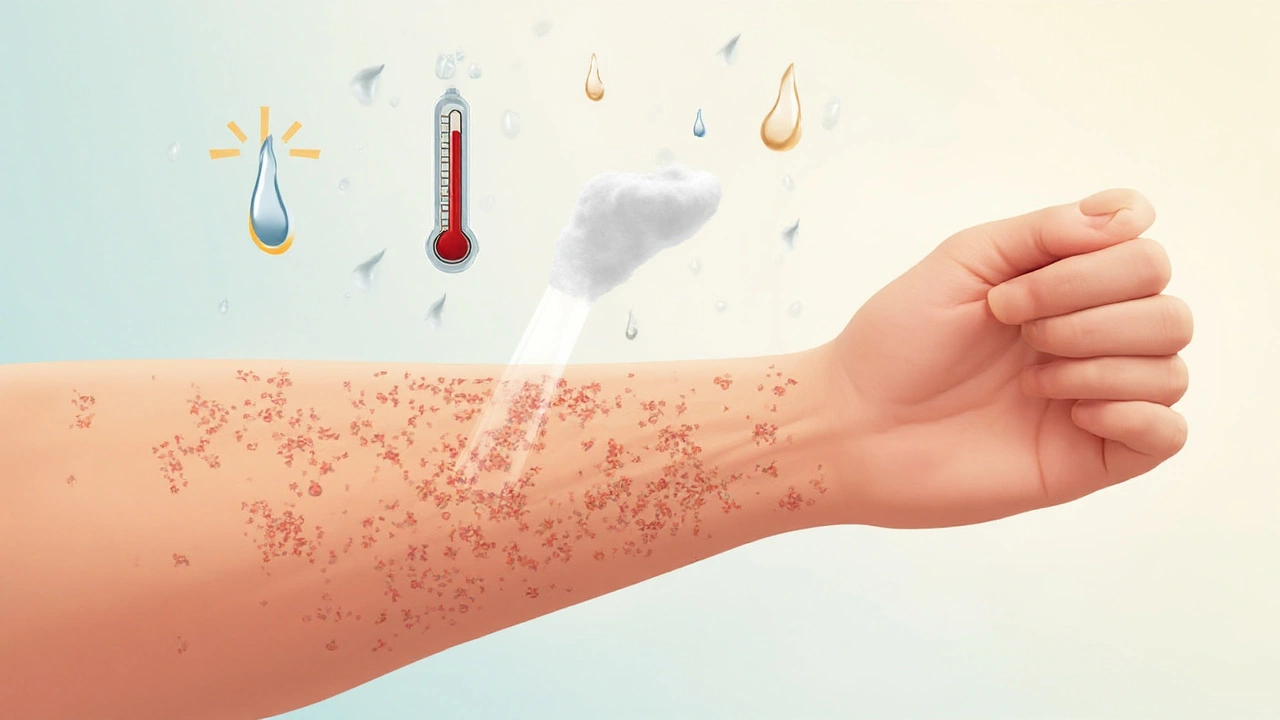
Fungal skin discoloration is a condition where the skin’s pigment shifts because of opportunistic fungi colonising the surface or deeper layers. The shift can appear as reddish, brownish, or even turquoise‑hued patches, depending on the species, depth of invasion, and how the body reacts. In most cases the colour change is a visible signal that the skin’s natural barrier and microbiome have been disrupted by external influences.
How fungi cause colour changes
Fungi such as dermatophytes keratin‑loving molds that thrive on dead skin, hair and nails produce enzymes that break down keratin, releasing pigments and inflammatory mediators. Candida species yeasts that prefer moist, warm environments and can infiltrate deeper epidermal layers trigger an immune response that leads to erythema and hyperpigmentation. Both groups feed off the same environmental conditions, which is why the surrounding climate and lifestyle matter more than the organism itself.
Key environmental drivers
Below are the most common factors that turn a harmless fungal presence into a visible discoloration.
- Humidity air moisture level, measured as relative humidity (RH) - When RH stays above 60% for prolonged periods, fungal spores germinate faster, producing more melanin‑like by‑products that tint the skin.
- Temperature ambient heat measured in degrees Celsius - Most pathogenic fungi grow optimally between 25°C and 30°C. Warm indoor heating or hot tubs create a perfect incubator.
- Excessive sweating hyperhidrosis that leaves the skin damp for hours - Sweat provides both moisture and salts that support fungal metabolism.
- Occlusive clothing tight, non‑breathable fabrics that trap heat and moisture - Think synthetic sportswear, leggings, or plastic‑coated shoes; they turn your skin into a humid micro‑climate.
- UV radiation sunlight or artificial UV that damages the skin barrier - UV can suppress local immunity, letting fungi proliferate, while also causing post‑inflammatory hyperpigmentation.
- Poor ventilation stagnant air in gyms, locker rooms, or bathrooms - Lack of airflow keeps moisture on surfaces, extending spore viability.
- Contaminated water chlorine‑poor pools, hot tubs, or untreated rainwater - Water that isn’t properly disinfected can harbour both dermatophytes and yeasts.
Comparing the two main fungal culprits
| Attribute | Dermatophytes | Candida |
|---|---|---|
| Typical species | Trichophyton rubrum, Microsporum canis | Candida albicans, Candida tropicalis |
| Preferred temperature (°C) | 25‑30 | 28‑35 |
| Common body sites | Feet, scalp, groin | Intertriginous folds, moist areas |
| Typical discoloration | Red to tan rings, sometimes brownish | Bright red patches, sometimes pink‑purple |
| Response to UV | Often suppressed | Can thrive after UV‑induced barrier loss |
How the skin microbiome fits into the picture
The skin microbiome the community of bacteria, fungi and viruses living on the epidermis acts like a protective fence. When humidity spikes or you wear tight shoes, the balance shifts: beneficial bacteria decline, while opportunistic fungi seize the chance. Studies from the UK Dermatology Society (2023) show a 40% rise in fungal discoloration cases during unusually wet summer months, correlating directly with reduced bacterial diversity.
Compounding personal factors
Even the perfect climate can’t save you if you have underlying issues. Immunosuppression a weakened immune system caused by medication, disease or age lowers the skin’s ability to ward off fungal overgrowth. Likewise, frequent use of topical antibiotics creams that kill bacteria but spare fungi erodes the protective bacterial layer, opening the door for discoloration.
Practical steps to keep fungal skin discoloration at bay
- Monitor indoor humidity - keep RH below 50% with a dehumidifier during damp seasons.
- Choose breathable fabrics - cotton, bamboo or moisture‑wicking synthetics let sweat evaporate.
- Dry thoroughly after showers or swimming - pay special attention to skin folds.
- Ventilate high‑moisture spaces - open windows, use exhaust fans in bathrooms and gyms.
- Limit UV over‑exposure - wear sunscreen and protective clothing; avoid tanning beds.
- Maintain a balanced skin microbiome - use mild, probiotic‑rich cleansers instead of harsh antibacterials.
- Check water quality - ensure pools and hot tubs have proper chlorine levels (≥1ppm).
Related concepts worth exploring
Understanding fungal skin discoloration opens doors to other skin‑health topics such as dermatophyte infections of nails, the role of hyperhidrosis excessive sweating that fuels fungal growth, and the impact of seasonal allergies which can inflame skin and make it more vulnerable. Readers may also want to dig into antifungal resistance the growing problem of fungi becoming less responsive to standard medications, especially if they’ve dealt with recurrent discoloration.

Frequently Asked Questions
What triggers fungal skin discoloration in winter?
Heating systems lower indoor humidity but also raise temperature, creating a warm, dry environment that encourages fungi on the skin surface. Closed‑off clothing and less ventilation add moisture from sweat, so the combination often leads to colour changes on the feet, groin and torso.
Can UV light cure fungal discoloration?
UV can kill some surface fungi, but it also damages the skin barrier and promotes post‑inflammatory hyperpigmentation. It’s generally safer to rely on topical antifungals and proper hygiene rather than sunlight as a treatment.
Why does my skin turn brown after a fungal infection?
The brown hue is usually melanin produced by skin cells in response to inflammation. Fungal enzymes can also generate pigmented metabolites that settle in the epidermis, leaving a lasting tint even after the infection clears.
How long does it take for discoloration to fade after treatment?
Visible fading typically occurs within 2‑4 weeks of effective antifungal therapy. Complete pigment normalisation may take up to 3 months, especially if the skin was heavily inflamed.
Are there natural remedies that prevent fungal discoloration?
Tea tree oil, apple cider vinegar and probiotic creams have shown modest success in lab studies. They work best as adjuncts to hygiene measures-not as stand‑alone cures.




20 Comments
The nexus between ambient humidity and fungal pigment production is a classic illustration of environmental microbiology; when relative humidity consistently exceeds sixty percent, we observe a marked escalation in spore germination, enzymatic activity, and consequently, the deposition of melanin‑like metabolites upon the epidermis, thereby imparting a spectrum of discoloration that ranges from ruddy scarlet to deep umber; such physiological cascades underscore the imperative for diligent indoor climate regulation, especially within residential and occupational settings where microclimatic conditions can be meticulously modulated through dehumidification, ventilation enhancement, and the strategic selection of breathable textiles, all of which serve to attenuate fungal proliferation and preserve cutaneous chromatic integrity.
Keep your skin dry and your home less humid, that’s all you need to stop those fungi from taking over.
It is fascinating how a simple shift in temperature by a few degrees can tip the balance in favor of dermatophytes; the thermodynamic window of twenty‑five to thirty degrees Celsius aligns perfectly with human comfort, yet it also provides an optimal incubator for these organisms. When we pair this with moisture-whether from sweat or ambient humidity-the metabolic pathways of fungi are super‑charged, leading to pigment production that manifests visibly on the skin. 🌿✨ Maintaining a stable micro‑environment is thus not merely a comfort issue, but a biochemical one.
Picture this: a sauna‑like atmosphere in your gym locker room, the air thick with sweat, and every breath you take is saturated with fungal spores. In that steamy crucible, the fungi unleash enzymes that break down keratin, releasing pigments that paint your skin in alarming hues. The drama isn’t just in the colour; it’s a battle between your immune defenses and the opportunistic microbes, each vying for dominance on the surface of your epidermis.
The discourse surrounding fungal skin discoloration often succumbs to a reductive dichotomy, wherein humidity is cast as the sole villain, yet this narrative neglects the intricate symphony of environmental and host factors that orchestrate the phenomenon. First, the hygroscopic nature of certain fabrics serves as a capillary conduit, drawing moisture to the skin's surface and fostering a microhabitat wherein spores not only survive but thrive, thereby amplifying enzymatic activity that yields chromogenic by‑products. Second, thermoregulation within indoor spaces, particularly those equipped with radiant heating, inadvertently establishes a thermal plateau of twenty‑five to thirty degrees Celsius-an optimal niche for both dermatophytes and Candida species-underscoring the paradox of comfort versus pathogen proliferation. Third, the physiologic response of hyperhidrosis introduces an excess of electrolytes, which function as co‑factors in fungal metabolism, further catalyzing pigment synthesis. Fourth, the occlusion resulting from synthetic attire imposes a barrier that restricts evaporative cooling, thereby maintaining a persistent state of dampness; this is not merely a passive condition but an active driver of microbial colonization. Fifth, ultraviolet radiation, while capable of diminishing surface fungal loads, simultaneously compromises the stratum corneum's barrier function, precipitating inflammatory cascades that culminate in post‑inflammatory hyperpigmentation-a dual‑edged sword that complicates therapeutic strategies. Sixth, ventilation deficits in communal spaces such as gyms and locker rooms produce stagnant air masses, which extend spore viability and increase the probability of inoculation upon skin contact. Seventh, the quality of water used for bathing or recreational activities cannot be overlooked; chlorination deficits permit fungal survival, turning pools into reservoirs of infection. Moreover, the host's immunologic landscape is a determinant of susceptibility; immunosuppressed individuals lack the cellular arsenal required to curtail fungal overgrowth, rendering them particularly vulnerable to both colonization and the ensuing pigmentary changes. Finally, the indiscriminate use of topical antibacterials erodes the commensal bacterial flora that ordinarily competes with fungi, thereby removing a critical line of defense. In sum, the etiologic tapestry is woven from a confluence of humidity, temperature, occlusion, UV exposure, ventilation, water quality, immunologic status, and microbial interplay, each thread demanding recognition in both preventative and therapeutic paradigms.
Great points! If you keep your environment dry and wear breathable fabrics, you’ll give your skin a huge advantage over those pesky fungi.
yeah, just crack a window and ditch the plastic sneakers, it'll help a ton.
I really appreciate the depth of the analysis provided earlier; it prompts a holistic view of how our daily habits intersect with microbial ecology. By acknowledging the role of moisture-whether from ambient humidity or our own perspiration-we can better tailor our personal hygiene routines. For instance, regularly changing socks and opting for cotton or bamboo socks can dramatically reduce the residual dampness that fuels fungal growth. Moreover, incorporating a post‑shower routine that emphasizes thorough drying of skin folds is a simple yet effective measure. When it comes to clothing, selecting moisture‑wicking fabrics that promote evaporation can interrupt the continuous moisture cycle that many dermatophytes rely upon. The environment at home also matters: using a dehumidifier in basements or bathrooms can lower relative humidity below the 60 % threshold often cited as a tipping point for spore germination. Finally, periodic monitoring of water quality in pools or hot tubs ensures that chlorine levels remain adequate to suppress fungal reservoirs. All these practical steps, when combined, form a comprehensive strategy to keep our skin’s microbiome balanced and resilient.
Sure, everyone can just follow those ‘simple’ steps, but have you ever considered that the very air we breathe is laced with hidden spores deliberately released by unseen forces to undermine our health? The ‘indoor humidity’ narrative is a convenient distraction from the broader agenda of population control through biological means.
Feeling frustrated about skin changes? You’re not alone, and a little empathy can go a long way 😊. Stay hopeful, and remember that many simple adjustments can make a big difference.
When we contemplate the mutable nature of skin pigmentation under fungal influence, we encounter a profound metaphor for existential flux; the epidermis, a canvas of identity, becomes a living palimpsest, continually rewritten by unseen biochemical authors. Each hue, whether crimson or cerulean, is a testament to the dynamic interplay between host defense mechanisms and microbial opportunism, inviting us to reflect on the impermanence of bodily constancy.
Just keep moving.
In light of recent findings regarding the thermodynamic preferences of dermatophytes, it is advisable to monitor ambient temperatures within domestic environments, ensuring they remain below the optimal fungal growth range; this practice, coupled with rigorous humidity control, constitutes a dual‑pronged approach to mitigating cutaneous discoloration.
hey, just remember to switch to cotton tees and give your skin a break from that plastic stuff, it really helps.
Seriously, if you keep ignoring basic hygiene, you’re just inviting the problem to get worse. 🙄 Stop making excuses and take action now.
Our nation’s health is at stake, and we must enforce strict standards on indoor climate control to protect citizens from fungal threats. Anything less is unacceptable.
Let’s stay positive, folks!!! Maintaining low humidity, using breathable fabrics, and keeping spaces ventilated are simple steps-everyone can do them; by implementing these practices, we create healthier environments and empower ourselves to combat fungal discoloration effectively!!!
Coach’s tip: Start your day by checking the humidity on your phone, then choose clothing that lets your skin breathe-small habits stack up into big results. Keep tracking progress, and celebrate each improvement!
Oh, great, another reminder that we need to drink enough water-because apparently staying hydrated magically prevents fungal pigments from showing up on our skin. Might as well add a daily mantra: ‘I am a fungus‑free superhero.’
For anyone looking to balance their skin’s microbiome, consider incorporating probiotic‑rich cleansers into your routine; they help maintain beneficial bacterial populations that naturally keep opportunistic fungi in check.