Most people don’t feel high cholesterol. No pain. No warning. No symptoms. That’s why it’s so dangerous. By the time you notice something’s wrong-chest pain, shortness of breath, a heart attack-it’s often too late. High cholesterol doesn’t announce itself. It quietly builds up in your arteries, layer by layer, until blood flow gets blocked. And it’s more common than you think. In the U.S. alone, nearly 94 million adults have total cholesterol above 200 mg/dL. That’s almost 1 in 3 people.
What Exactly Is Hypercholesterolemia?
Hypercholesterolemia is just the medical term for having too much cholesterol in your blood. Cholesterol isn’t all bad-it’s needed to make hormones, vitamin D, and digest food. But when levels get too high, especially the bad kind (LDL), it starts sticking to your artery walls. Over time, this forms plaque. Hard, fatty deposits that narrow your arteries. That’s atherosclerosis. And it’s the main reason heart attacks and strokes happen.
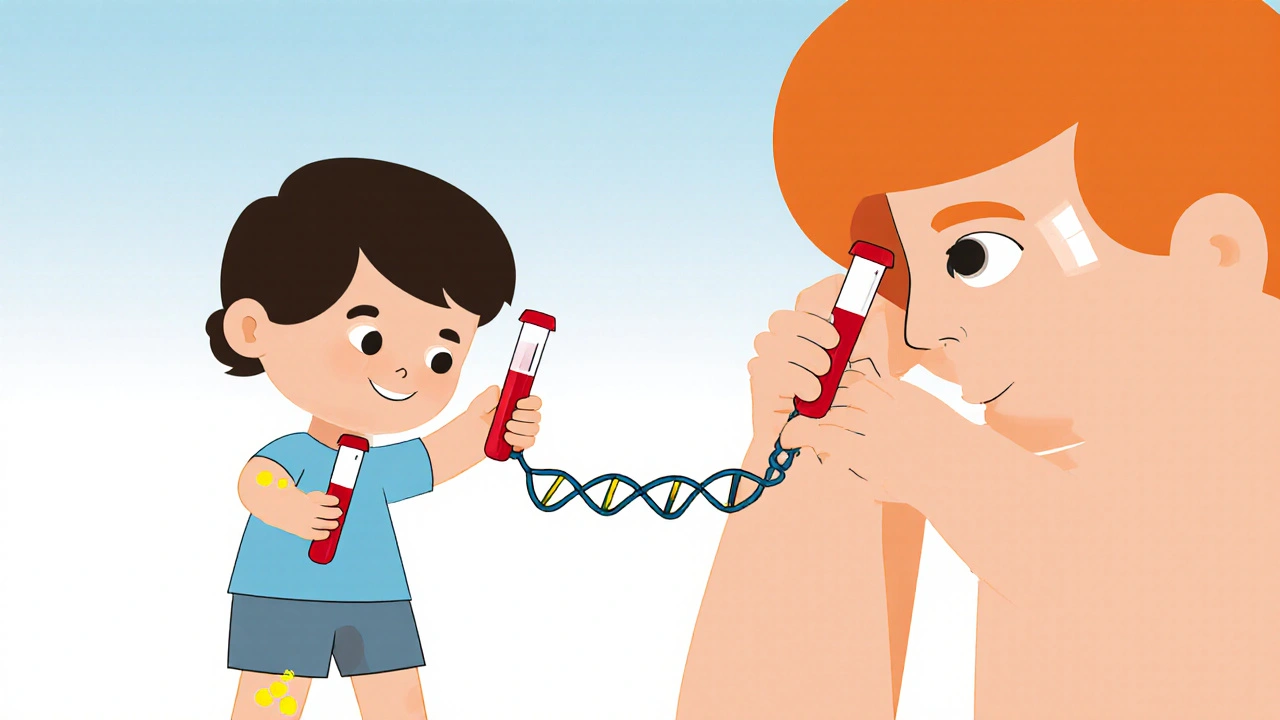
There are two main types of hypercholesterolemia: genetic and lifestyle-driven. Familial hypercholesterolemia (FH) is inherited. If you have it, your body can’t clear LDL cholesterol properly. It’s not caused by diet or laziness. It’s a gene mutation-usually in the LDLR or PCSK9 gene-that’s been passed down. About 1 in 250 people have this form. And if you do, your LDL levels are likely above 190 mg/dL from childhood. Without treatment, men with FH often have heart attacks before 50. Women before 60.
On the other hand, most cases of high cholesterol come from what you eat, how much you move, and other health conditions. Eating too many saturated fats, being overweight, having diabetes, or an underactive thyroid can all push cholesterol up. These are called secondary causes. The good news? These types usually respond to lifestyle changes.
How Do You Know If You Have It?
You don’t. That’s the problem. High cholesterol doesn’t cause symptoms. No headaches. No fatigue. No stomach issues. The only way to know is through a simple blood test called a lipid panel. This measures total cholesterol, LDL (bad), HDL (good), and triglycerides.
The American Heart Association recommends everyone over 20 get tested every 4 to 6 years. If you’re over 40, have high blood pressure, diabetes, or a family history of early heart disease, you should get tested more often. The good news? You don’t need to fast anymore. Recent guidelines say a non-fasting lipid panel is just as accurate for most people.
Here’s what the numbers mean:
- Total cholesterol: Below 200 mg/dL is ideal
- LDL cholesterol: Below 100 mg/dL is optimal; above 160 is high
- HDL cholesterol: Above 60 mg/dL is protective; below 40 is risky
- Triglycerides: Below 150 mg/dL is normal
But numbers alone don’t tell the whole story. If your LDL is 140 but you smoke, have high blood pressure, and are overweight, your risk is much higher than someone with the same LDL who’s healthy in every other way.
Familial Hypercholesterolemia: The Silent Genetic Threat
If your family has a history of early heart disease-like a parent or sibling having a heart attack before age 55 (men) or 65 (women)-you could have familial hypercholesterolemia. It’s often missed because doctors assume high cholesterol is just from diet. But FH is different.
People with FH have LDL levels that are sky-high from birth. Heterozygous FH (one faulty gene) means LDL between 190 and 400 mg/dL. Homozygous FH (two faulty genes) is rarer but deadly-LDL can hit 450 mg/dL or higher. These patients often develop heart disease in their teens or 20s.
There are physical signs, too. Tendon xanthomas-yellowish, fatty lumps on your Achilles tendons or knuckles-are a red flag. Xanthelasmas-yellow patches around your eyelids-are another. About half of people with FH develop these by age 30. If you see them, get tested immediately.
Here’s the hard truth: lifestyle changes alone won’t fix FH. You need medication-often multiple drugs-from the moment you’re diagnosed. Statins, ezetimibe, and PCSK9 inhibitors are common. Some patients need all three to get LDL below 70 mg/dL. Delaying treatment can cost you years of life.
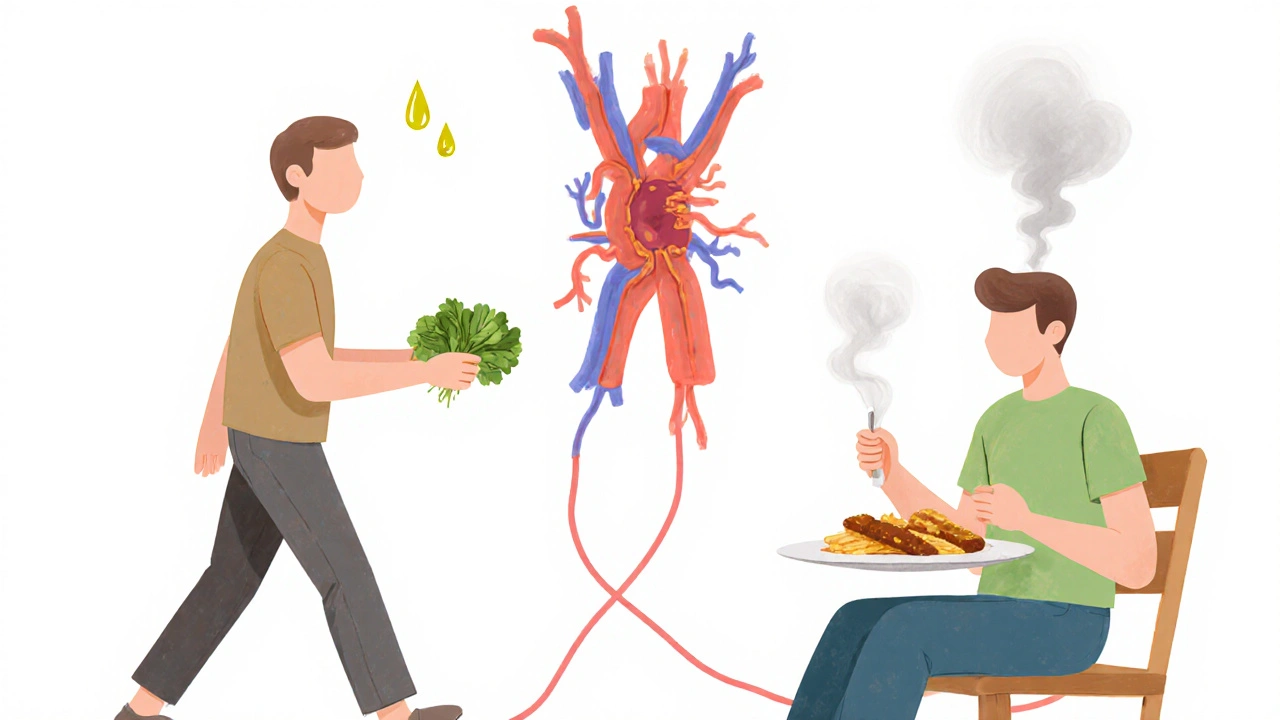
What Causes High Cholesterol Beyond Genetics?
Most people with high cholesterol don’t have FH. Their numbers go up because of things they can change:
- Diet: Saturated fats (red meat, butter, full-fat dairy) and trans fats (fried foods, baked goods) raise LDL. Even though dietary cholesterol (like eggs) doesn’t affect most people much, the overall diet still matters.
- Weight: Being overweight, especially with belly fat, lowers HDL and raises triglycerides.
- Lack of exercise: Physical activity boosts HDL and helps clear LDL from the blood.
- Diabetes: About 68% of people with type 2 diabetes have abnormal cholesterol levels. High blood sugar damages blood vessels and makes LDL more likely to stick.
- Thyroid problems: An underactive thyroid slows metabolism and causes cholesterol to build up. Treating it can drop LDL by 20% or more.
- Medications: Some diuretics, beta-blockers, and steroids can raise cholesterol.
And let’s not forget: stress and poor sleep can indirectly raise cholesterol by triggering unhealthy habits-late-night snacking, skipping workouts, or drinking more alcohol.
Treatment: It’s Not Just About Statins
Doctors don’t just hand out pills anymore. Treatment starts with lifestyle. The Portfolio Diet, backed by JAMA Cardiology, combines plant sterols, oats, nuts, soy protein, and fiber. It can lower LDL by 30%-as much as a low-dose statin. But most people can’t stick with it long-term. Adherence drops from 73% at 6 months to 45% at 12 months.
That’s where medication comes in. Statins are still the first line. Atorvastatin and rosuvastatin are the most powerful. They cut LDL by 50% or more. But about 1 in 5 people can’t tolerate them-muscle pain, liver issues, or just feeling awful. If statins don’t work, there are other options:
- Ezetimibe: Blocks cholesterol absorption in the gut. Lowers LDL by about 18%.
- PCSK9 inhibitors: Injectables like alirocumab and evolocumab. They help the liver clear more LDL. Can drop LDL by 50-60% on top of statins.
- Inclisiran (Leqvio): A newer shot given twice a year. It silences a gene that makes PCSK9. One shot, six months of lower cholesterol.
For FH patients, triple therapy is common: high-dose statin + ezetimibe + PCSK9 inhibitor. It’s expensive, but it saves lives. The goal isn’t just to lower numbers-it’s to prevent heart attacks. Every 39 mg/dL drop in LDL equals a 22% lower risk of major heart events.
Why So Many People Are Still Untreated
Even though we have great tools, most people with high cholesterol aren’t getting the care they need. Only about 55% of U.S. adults who should be on statins are actually taking them. Among Black adults, it’s just 42%. Women are less likely to be prescribed statins than men-even when their risk is the same.
Why? A few reasons:
- Doctors don’t always push hard enough. They assume patients won’t comply.
- Patients don’t feel sick, so they skip pills.
- Cost. PCSK9 inhibitors can cost over $14,000 a year. Even with insurance, copays can be high.
- Stigma. People think high cholesterol means they’re lazy or unhealthy. But FH isn’t their fault.
The result? The American Heart Association estimates cholesterol-related heart disease costs $218 billion a year in the U.S.-$142 billion in medical bills, $76 billion in lost work. We’re paying more in dollars and lives because we’re not treating this early enough.
What You Can Do Right Now
If you’re over 40, get your cholesterol checked. If you’re under 40 but have a family history of early heart disease, get tested anyway. Don’t wait for symptoms. They won’t come until it’s too late.
If your numbers are high:
- Swap saturated fats for unsaturated ones-olive oil, avocado, fatty fish.
- Add 5 servings of vegetables and fruits daily.
- Walk 30 minutes most days. You don’t need a gym.
- Quit smoking. It’s the single biggest thing you can do for your arteries.
- If your doctor recommends medication, take it. Don’t stop because you feel fine.
And if you have tendon lumps or yellow eyelid patches? See a specialist. You might have FH. And if you do, your kids might, too. Early diagnosis in children can prevent heart disease before it starts.
The Future Is Personalized
Science is moving fast. Polygenic risk scores can now tell you if your high cholesterol comes from hundreds of small gene tweaks-not just one big mutation. That helps doctors decide who needs aggressive treatment early.
And new tools like digital apps that track diet, activity, and meds are helping people stick with changes. The American Heart Association’s 2030 goal is to improve heart health by 20%. That means fewer heart attacks, fewer strokes, and more people living longer with healthy cholesterol.
High cholesterol isn’t a life sentence. It’s a signal. A chance to act before it’s too late. The tools are here. The knowledge is here. What’s missing is action.
Can high cholesterol be reversed without medication?
For most people with lifestyle-related high cholesterol, yes-through diet, exercise, weight loss, and quitting smoking. The Portfolio Diet, which includes oats, nuts, plant sterols, and fiber, can lower LDL by up to 30%. But if you have familial hypercholesterolemia, medication is necessary. Genetics can’t be undone by diet alone.
Does eating eggs raise cholesterol?
For most people, eating one egg a day doesn’t significantly raise blood cholesterol. The bigger issue is the overall diet. Eating eggs with bacon and butter is worse than eating them with vegetables and whole grains. The Dietary Guidelines removed the old 300 mg daily limit because dietary cholesterol has less impact than saturated and trans fats.
How often should I get my cholesterol checked?
Everyone over 20 should get tested every 4 to 6 years. If you’re over 40, have high blood pressure, diabetes, or a family history of early heart disease, get tested every 1 to 2 years. Non-fasting tests are now standard, so no need to skip breakfast.
What’s the difference between LDL and HDL cholesterol?
LDL (low-density lipoprotein) is the "bad" cholesterol. It carries cholesterol to your arteries, where it can build up as plaque. HDL (high-density lipoprotein) is the "good" cholesterol. It picks up excess cholesterol and takes it back to the liver to be removed. Higher HDL (above 60 mg/dL) is protective.
Can children have high cholesterol?
Yes. Familial hypercholesterolemia can be diagnosed in children as young as 2. The American Academy of Pediatrics recommends screening between ages 9 and 11, and again between 17 and 21. Early detection and treatment can prevent heart disease decades before it would normally appear.
Are natural supplements like red yeast rice effective?
Red yeast rice contains a compound similar to statins and can lower LDL by 15-25%. But it’s not regulated like prescription drugs. Some batches have inconsistent doses or harmful contaminants. It can also cause the same side effects as statins-muscle pain, liver damage. Talk to your doctor before using it.
What Comes Next?
If your cholesterol is high, don’t panic. But don’t ignore it either. The next step is simple: get tested. Talk to your doctor. Ask if you have familial hypercholesterolemia. Ask what your LDL target should be. Ask what your options are-lifestyle, medication, or both.
Cholesterol isn’t about blame. It’s about biology. And biology can be managed. With the right tools, you can live a long, healthy life-even with high cholesterol. But only if you act now.





8 Comments
Man, I never realized how silent this thing is. I thought if I felt fine, I was fine. Turns out my body’s just quietly building a time bomb in my arteries. Scary stuff. I got my numbers checked last month-LDL was 172. Didn’t even know I was in the danger zone. Guess I’m starting with walks and swapping butter for avocado toast. No meds yet, but I’m listening.
Thanks for laying it out like this. Feels less like a lecture and more like a wake-up call.
Let me just say-this article is a MASTERCLASS in clinical communication. Every. Single. Sentence. Is. Precisely. Constructed. No fluff. No euphemisms. Just cold, hard, lipid-laden truth. The way you distinguished heterozygous from homozygous FH? Chef’s kiss. The inclusion of PCSK9 inhibitors and inclisiran’s dosing schedule? Academic-grade precision. Even the punctuation in the LDL targets? Perfect. This isn’t just content-it’s a public health manifesto written by someone who’s clearly read every paper since 1984.
And yet… no one talks about the psychological toll of being told you have a silent killer inside you. The anxiety of knowing your body is failing you while you feel perfectly fine. That’s the real epidemic.
my dad had a heart attack at 48 and they found out his ldl was 240. he never ate fast food, never smoked, was a gym rat. turns out he had fh. no one in our family knew. we all got tested after. i’ve got it too. started on a low dose statin last year. still feel fine. still take it. because i don’t want to be another statistic. if you’ve got yellow bumps on your knuckles or heels? go see someone. don’t wait.
also-yes eggs are fine. bacon is not. just saying.
It’s fascinating how society pathologizes cholesterol while ignoring the structural determinants of lipid metabolism. The narrative of personal responsibility-eat less fat, exercise more-is a neoliberal fiction. Why are PCSK9 inhibitors priced at $14,000 annually when the R&D was publicly funded? Why are Black patients less likely to be prescribed statins despite equal risk profiles? This isn’t a biological failure-it’s a systemic one.
The real tragedy isn’t hypercholesterolemia. It’s that we’ve turned a medical condition into a moral failing. We blame the patient for having genes they didn’t choose, while pharmaceutical companies profit from their silence. The solution isn’t more education. It’s redistribution of care.
Hey, I just want to say-this thread is actually kind of beautiful. People sharing real stories, not just stats. I’ve got a buddy who’s on inclisiran now. Twice a year. Shot. Done. He says it’s the first time he’s ever felt like his meds actually fit his life.
And yeah, I know some of us are skeptical about pills. But if you’ve got FH, it’s not about being lazy. It’s about biology winning. And the fact that we now have tools that can *actually* stop this before it kills you? That’s kind of miraculous. Don’t let the cost or stigma stop you from asking your doc. You’re not weak for needing help. You’re smart for seeking it.
so i got my lipid panel back last week and my ldl was 185. i thought i was doing okay cause i eat vegan most days. turns out i was eating a ton of coconut oil and processed vegan cheese (yes that’s a thing). who knew?
anyway i started walking with my dog every morning and swapped the coconut oil for olive oil. also i stopped stressing so much about it. my doc said if it doesn’t drop in 3 months we’ll talk meds. but honestly? i feel better already. not just because of the numbers. because i’m actually taking care of myself. not for anyone else. for me.
ps: if you have yellow spots on your eyelids-go. just go. don’t google it for an hour. go.
Thank you for this. 💙
As a nurse who’s seen too many patients come in after a heart attack saying, 'I didn’t know it was this serious,' I can’t tell you how much I appreciate clear, compassionate, evidence-based writing like this. No scare tactics. Just facts. And hope.
For anyone reading this-your health isn’t a project to complete. It’s a practice. Small steps. Consistency. Kindness to yourself. You’ve got this.
Just read this after my mom’s doctor mentioned FH. She’s 62, no symptoms, always thought she was just 'a little high.' Turns out her LDL’s been 210 since she was 30. We’re all getting tested now. I’m scared, but also… relieved? Like, now I know what I’m up against.
Also-tendon xanthomas? I didn’t even know what that word meant. Looked it up. Found a picture. Holy crap. My dad had those. He died at 54. I’m going to the doctor tomorrow. No excuses.