What Is Corticosteroid-Induced Hyperglycemia?
When you take corticosteroids like prednisone, dexamethasone, or hydrocortisone for inflammation, asthma, or autoimmune diseases, your blood sugar can spike-even if you’ve never had diabetes before. This isn’t just a side effect. It’s a real metabolic condition called corticosteroid-induced hyperglycemia, and in up to 32% of patients, it turns into full-blown steroid-induced diabetes.
Unlike type 2 diabetes, which develops slowly over years, this happens fast. Within hours of taking your first dose, your body starts resisting insulin, your liver dumps out more glucose, and your pancreas struggles to keep up. A single 75 mg dose of prednisolone can shut down insulin production in less than two hours. By the next morning, your blood sugar might be 200 mg/dL or higher-without you even eating anything.
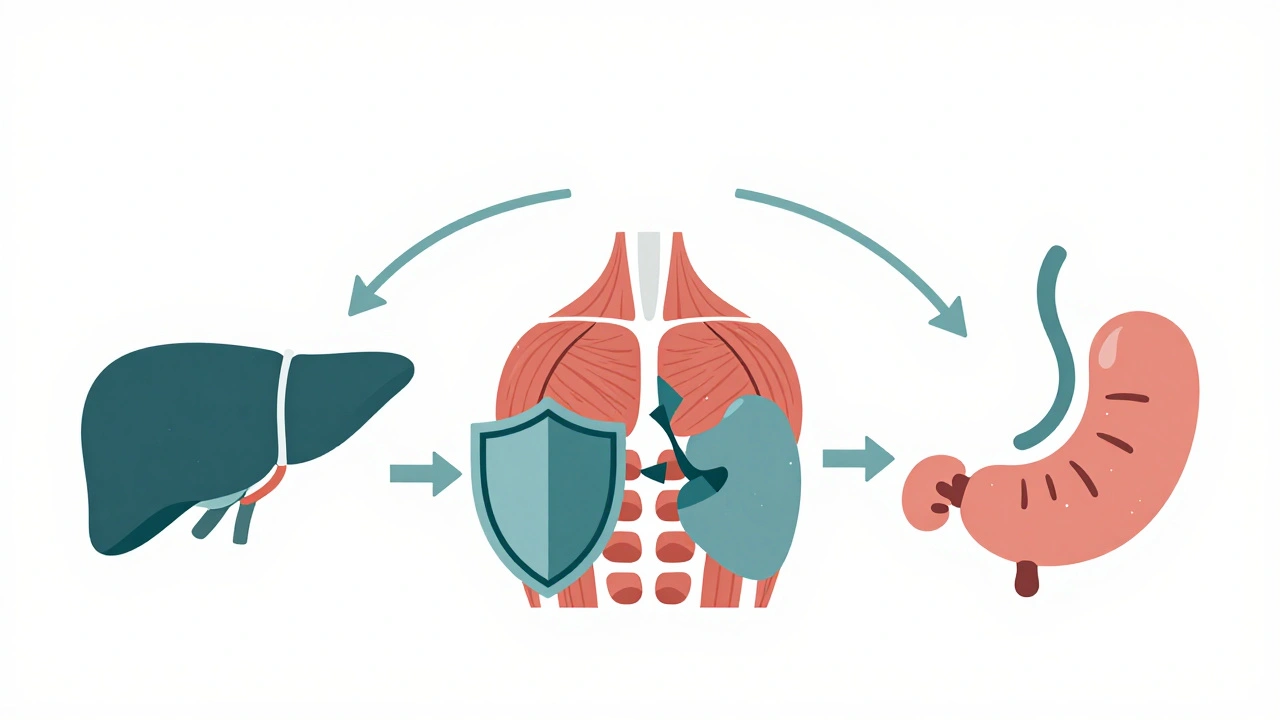
Why Does This Happen?
It’s not just one thing. Corticosteroids attack your metabolism from multiple angles.
- In your liver, they crank up glucose production by nearly 38%, turning on enzymes that make sugar from scratch.
- In your muscles, they block the glucose transporters (GLUT4) that pull sugar out of your blood-reducing uptake by over 40%.
- In your fat tissue, they break down stored fat, flooding your bloodstream with free fatty acids that make insulin even less effective.
- In your pancreas, they silence the cells that make insulin, cutting down key receptors like GLUT2 and glucokinase.
These changes don’t happen all at once. Insulin resistance starts 4 to 6 hours after a dose and lasts over 16 hours. But here’s the twist: your blood sugar doesn’t stay high all day. It peaks in the morning, drops by afternoon, and sometimes crashes at night-especially when you start tapering off. That’s why fingerstick tests at random times miss half the problem.
Who’s at Risk?
Not everyone gets high blood sugar on steroids. But some people are far more likely to.
- People with a BMI over 30 are 3.2 times more likely to develop hyperglycemia.
- If you already have prediabetes or impaired glucose tolerance, your risk jumps 4.7 times.
- Those on doses higher than 20 mg of prednisone daily are at the highest risk.
- Older adults and people with a family history of diabetes are also more vulnerable.
It’s not just about the dose. The type matters too. Dexamethasone is stronger and longer-lasting than hydrocortisone, so it causes more severe spikes. Even short courses-like a 5-day burst for a flare-up-can trigger dangerous highs.
How to Monitor Blood Sugar Correctly
Waiting for symptoms like thirst or fatigue means you’re already too late. You need to check blood sugar before it becomes a crisis.
The American Diabetes Association and Endocrine Society agree: start monitoring within 24 hours of your first steroid dose. For high-risk patients, test fasting and 2 hours after each meal-twice a day minimum. But here’s what most hospitals still get wrong: they only test in the morning.
That’s not enough. Because steroid-induced hyperglycemia follows a sharp morning peak, you need to test after breakfast, lunch, and dinner. And if you’re on an alternate-day schedule, test on both steroid and non-steroid days. Insulin resistance lingers for 16 to 24 hours after the last dose.
Continuous glucose monitors (CGMs) catch 68% more high blood sugar events than fingersticks alone. They’re especially useful at night, when 23% of patients drop into dangerous lows during steroid tapering. A patient might feel fine during the day but wake up sweating, shaky, and confused because their sugar crashed overnight.
How to Treat It-Without Stopping Steroids
You can’t just stop the steroid. It’s often lifesaving. So treatment must work around it.
For patients with pre-existing diabetes, insulin doses usually need to go up by 20% to 50%. But for new-onset steroid diabetes, sliding scale insulin (giving insulin only when sugar is high) fails 60% of the time. Why? Because it’s reactive, not proactive.
The gold standard is basal-bolus insulin: a long-acting insulin once a day (like glargine or degludec) to cover background needs, plus rapid-acting insulin before meals to match the steroid spike. Dosing should be timed to the steroid schedule. If you take prednisone at 8 a.m., your biggest insulin dose should be at breakfast. Lunch and dinner doses are smaller. At night, you might need almost no insulin-unless you’re tapering.
Oral diabetes drugs? Metformin helps a little with insulin resistance, but it won’t fix the insulin shortage. SGLT2 inhibitors and GLP-1 agonists are risky-they can cause dehydration or ketoacidosis in steroid users. Insulin is still the only reliable tool.
What Happens If You Don’t Manage It?
High blood sugar from steroids doesn’t just cause discomfort. It can kill.
Each year, 4.7% of severe cases lead to hyperglycemic hyperosmolar state-a life-threatening dehydration and confusion syndrome. Another 2.3% develop diabetic ketoacidosis, even without type 1 diabetes. These are ICU-level emergencies.
Longer term, uncontrolled sugar during steroid treatment increases the risk of infections, delayed wound healing, and longer hospital stays. One study found patients with unmanaged steroid-induced hyperglycemia stayed in the hospital 1.8 days longer than those whose sugar was controlled. That’s over $2,300 extra per person in costs.
And here’s the scary part: even after you stop steroids, some people never fully recover. About 1 in 5 develop permanent type 2 diabetes within a year. That’s why monitoring doesn’t stop when the last pill is taken.

Why Most Hospitals Fail at This
Despite clear guidelines, only 58% of non-ICU hospital units have written protocols for steroid-induced hyperglycemia. That means many nurses don’t know when to test, and doctors don’t know when to start insulin.
One study found that 32% of treatment errors happened because insulin was given at the wrong time-like giving a big dose at night when the steroid effect had already worn off. Another 44% of non-endocrinology doctors couldn’t identify the classic morning spike pattern.
Places that did it right-like Mayo Clinic-saw complications drop by over 50%. Their protocol? Test glucose within 4 hours of the first steroid dose. Start insulin if two readings hit 180 mg/dL or higher. Train every nurse and pharmacist. Make it part of the admission checklist.
What’s Coming Next
Research is moving fast. The NIH is testing a machine learning tool that predicts your personal risk based on your BMI, HbA1c, steroid dose, and even a gene variant called GR-1B. Early results show 84% accuracy.
Drug companies are working on new steroids that don’t wreck your metabolism. These so-called “steroid-sparing” drugs and selective glucocorticoid receptor modulators are in Phase II trials. They aim to fight inflammation without raising blood sugar.
For now, the best defense is awareness. If you’re prescribed corticosteroids, ask: “Will I need my blood sugar checked? What’s the plan if it goes high?” Don’t assume it’s just a routine side effect. It’s a medical event-and it’s preventable.
What Patients Say
Over 1,200 patients surveyed by the American Diabetes Association described their experience as a “rollercoaster.” Many reported sudden lows during tapering-sometimes so bad they passed out. Others were told their high sugar was just “stress,” not the steroid. Some were discharged without any follow-up plan.
One patient wrote: “I was on prednisone for 2 weeks. My sugar went from 90 to 280. They gave me insulin but never told me what to do when I stopped. Two days later, I was dizzy and sweating. I thought I was having a heart attack. It was low blood sugar.”
Education matters. Patients who got a printed plan with glucose targets, insulin timing, and warning signs had 70% fewer emergency visits.




12 Comments
Okay, so I’ve been managing steroid-induced hyperglycemia for my mom for the past 8 months now-she was on a 3-week prednisone burst for polymyalgia, and honestly? It was a nightmare. We didn’t know to test after meals, only fasting, and she kept crashing at night. By week two, she was waking up drenched in sweat, confused, thinking she was having a stroke. Turns out, her BG dropped to 52. CGM saved her life. I wish someone had told us about the 16-hour insulin resistance window. Now we test pre-breakfast, post-breakfast, pre-lunch, post-lunch, and bedtime. Even on non-steroid days. The morning spike is real. And yes, insulin is the only thing that works. Oral meds? Useless. Sliding scale? A joke. Basal-bolus is non-negotiable. Also, tapering is the silent killer. Don’t assume it’s over when the pills stop.
This is such an important post. I’m a nurse in a med-surg unit, and we still don’t have a standardized protocol. We test fasting, sometimes post-prandial if we remember. But I’ve seen patients crash because we gave insulin at night when the steroid effect had already worn off. It’s not negligence-it’s lack of training. I printed out the ADA guidelines and posted them on our unit board. One of the residents actually thanked me. Maybe change starts small. If you’re on steroids, ask for a glucose log. Don’t wait to be told.
bro this is wild 😳 i was on prednisone for a rash last year and my sugar went from 95 to 240 in 2 days. no idea why i was so thirsty all the time. they gave me insulin but never said anything about when to take it or what to do when i stopped. i thought i was just ‘stressed.’ turns out i was having lows at 3am. i’m still scared to even think about steroids again. pls tell me i’m not the only one?
i had this happen to me too!! i was on 40mg prednisone for 10 days and my dr just said ‘watch your sugar’ but never gave me a plan. i checked once a day and thought i was fine. then i passed out at the grocery store. turned out i was at 48. they said it was ‘low blood sugar from tapering’ but no one warned me. please someone tell me if this is normal??
Yes, this is SO common and so under-discussed. I’m a pharmacist and I’ve had patients come in confused because their insulin was ‘taken away’ after they stopped steroids. They don’t realize insulin resistance lingers. I always give them a printed sheet: ‘When you stop steroids, don’t stop monitoring. Your body is still recovering.’ We even make little cards for patients: ‘Morning spike? Insulin. Night crash? Check sugar before bed. Tapering? Still test.’ Small things save lives.
Let’s be real-this is just Big Pharma’s way of keeping you dependent on insulin. They know steroids cause hyperglycemia, so they profit off the insulin sales. Why not just give people metformin and call it a day? Why force insulin? And why are CGMs so expensive? Someone’s making money off your suffering. This isn’t medicine-it’s a cash grab. You’re being manipulated.
Thank you for sharing this. I’ve been reading through all the comments and I just want to say-you’re not alone. I’ve had two family members go through this, and the lack of communication from medical teams was terrifying. One was discharged with no follow-up. The other was told ‘it’ll go away’-but it didn’t. I’ve started a small support group for steroid-induced diabetes. We share glucose logs, insulin timing tips, and emergency contacts. If you’re reading this and feel lost-DM me. I’ll send you our template. You don’t have to figure this out alone.
I’ve been in ICU for 18 months now because of steroid-induced DKA. I was on 60mg prednisone for a rare autoimmune condition. No one warned me. No one tested me properly. I was told ‘it’s just inflammation’ and sent home. Three days later, I was in the ER with a pH of 6.8. My kidneys failed. My brain swelled. I’m on dialysis now. And the doctors? They acted like it was my fault for not ‘monitoring better.’ I didn’t even know what ‘monitoring’ meant. This isn’t a side effect-it’s a medical crime. And nobody gets punished.
So let me get this straight-your body gets hijacked by a synthetic hormone, and instead of fixing the root cause, you just pump insulin into it? And you call this medicine? What if the whole concept of ‘blood sugar’ is just a capitalist construct? What if insulin resistance is your body’s way of saying ‘stop poisoning me with steroids’? Why are we treating the symptom instead of asking why we’re giving these drugs in the first place? The FDA is corrupt. The AMA is bought. And you’re all just drinking the Kool-Aid.
As someone who actually studied endocrinology at Johns Hopkins (unlike the majority of you commenting here), I find this post… mildly informative but deeply lacking in nuance. You’re ignoring the role of circadian cortisol rhythms in steroid-induced hyperglycemia. The morning spike isn’t just about timing-it’s about receptor downregulation in the hypothalamus. Also, you’re misrepresenting SGLT2 inhibitors. In low-dose steroid regimens, they’re perfectly safe with proper hydration. And why are you still using ‘basal-bolus’? That’s 2008 thinking. We’re now using closed-loop insulin pumps with predictive algorithms that adjust for steroid half-life. You’re all still living in the analog age.
It is a moral imperative to acknowledge that the systemic failure to implement standardized glucose monitoring protocols for patients on corticosteroids constitutes a profound dereliction of ethical duty by the medical establishment. The commodification of insulin, coupled with the institutionalized negligence of non-endocrinology providers, reflects a deeper epistemological collapse in contemporary clinical practice. One must ask: if a patient’s metabolic integrity is sacrificed for the expediency of anti-inflammatory therapy, then what, precisely, is the moral foundation of our therapeutic interventions? The answer, I fear, is none.
Just to add a real-world clinician’s take: in our hospital, we now have a ‘Steroid Glucose Protocol’ on the EHR. It auto-populates a glucose monitoring order when prednisone >20mg or dexamethasone >4mg is ordered. Nurses get a pop-up: ‘Test fasting, post-breakfast, post-dinner.’ If two readings >180, insulin order triggers automatically. We’ve cut DKA admissions by 60%. Also-CGM on discharge for anyone on >7 days of steroids. It’s not fancy. It’s just done. Stop treating this like an exception. It’s the rule.