When your knees ache after walking the dog, or your fingers stiffen up in the morning, it’s easy to write it off as "just getting older." But osteoarthritis isn’t normal aging-it’s a disease. And it’s not just about worn-out cartilage. It’s a whole-joint problem: bone thickens, ligaments tighten, and inflammation creeps in quietly, long before X-rays show damage. If you’re one of the 32.5 million American adults with osteoarthritis, or you’re watching a parent struggle with it, you’re not alone. The good news? You can take back control-even if the damage is already there.
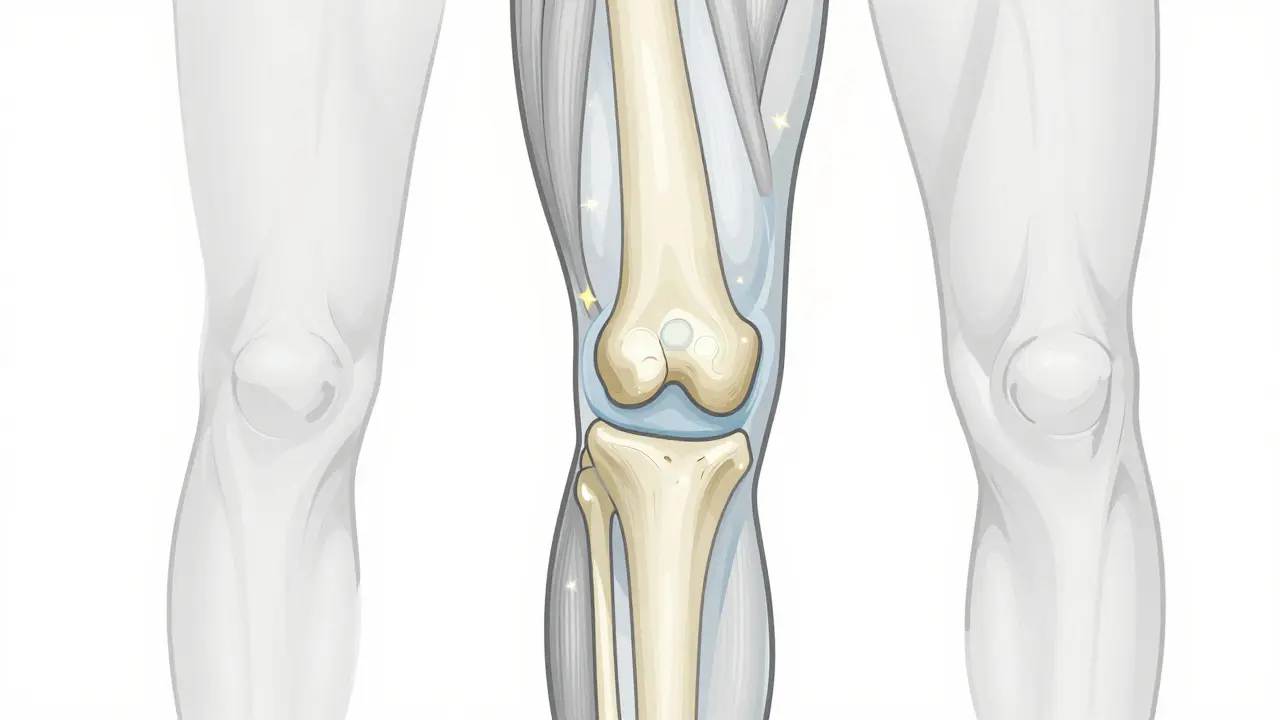
What’s Really Happening Inside Your Joint?
Osteoarthritis starts with cartilage, the smooth, rubbery tissue that cushions the ends of your bones. But it doesn’t stop there. As cartilage breaks down, the bone underneath starts to change. It thickens, forms bony spurs (osteophytes), and loses its normal shape. The synovial fluid that lubricates the joint gets thinner. Ligaments and tendons stretch or tighten, pulling the joint out of alignment. Fat tissue around the joint even releases inflammatory chemicals. This isn’t just friction from use-it’s a biological breakdown where repair can’t keep up with damage.
Unlike rheumatoid arthritis, where your immune system attacks your joints, osteoarthritis is driven by mechanical stress and biological imbalance. Repetitive motion, past injuries, or excess weight overload the joint. The body tries to fix it, but the repair process goes wrong. Chondrocytes-the cells that maintain cartilage-start producing enzymes that chew up the very tissue they’re supposed to protect. It’s a cycle: damage causes inflammation, inflammation causes more damage.
Some joints are more vulnerable. Knees take the brunt-60% of cases. Hips follow at 30%, hands at 25%, and spine at 20%. And it’s rarely symmetrical. One knee hurts more than the other. One hand stiffens while the other works fine. That’s because it’s not just age-it’s how you’ve used your body.
Why Pain Gets Worse (and Why Rest Doesn’t Fix It)
People often think if they stop moving, the pain will go away. But that’s the opposite of what works. OA pain flares with activity-climbing stairs, standing too long, carrying groceries-but it doesn’t vanish with rest like it does in rheumatoid arthritis. Instead, it lingers. Why? Because movement keeps the joint lubricated and strengthens the muscles that support it. When you avoid activity, muscles weaken, joints become stiffer, and pain actually increases.
Early on, pain comes and goes. You might feel it after gardening, then be fine the next day. But over time, the pain becomes constant. You wake up stiff. You can’t bend down to tie your shoes. Sleep gets ruined. A 2022 Arthritis Foundation survey found 68% of OA patients said pain interfered with sleep. That’s not just discomfort-it’s a life-altering burden.
And here’s the hidden trap: avoiding movement leads to weight gain, which puts more pressure on your joints. That leads to less movement. That leads to more pain. It’s a downward spiral the World Health Organization calls a "vicious cycle"-one that can also increase your risk of heart disease, diabetes, and depression.
What Actually Works: The Science-Backed Four-Pillar Approach
There’s no magic pill. But decades of research show that four strategies work together to slow progression and reduce pain:
- Weight loss - Losing just 10% of your body weight cuts knee pain by 50% in many cases. A 2023 study in the Journal of Orthopaedic & Sports Physical Therapy showed that people who lost 10 pounds or more improved their ability to walk 20% faster and with 40% less pain. It’s not about being thin-it’s about reducing load. Every extra pound adds 4 pounds of pressure on your knees.
- Exercise - Not just walking. You need strength training, flexibility work, and low-impact cardio. A 2022 Arthritis Foundation trial found that patients who did 45 minutes of land-based exercise three times a week for 12 weeks saw pain drop by 40% and function improve by 35%. Strength training matters most-quadriceps and glutes support your knees. Tai Chi and water aerobics are great for stiffness. Don’t wait for pain to disappear to start. Start moving, even if it’s slow.
- Physical therapy - A certified physical therapist teaches you how to move without hurting. They don’t just give you exercises-they correct your posture, teach joint protection techniques, and adjust your daily habits. Six to eight sessions can make the difference between managing pain and being crippled by it. Many patients report they didn’t realize they were walking wrong until a therapist showed them.
- Education - Knowing what you’re dealing with changes everything. The CDC’s 6-week self-management course cuts pain by 40% and improves function by 30%. It’s not about memorizing anatomy-it’s about learning how to pace yourself, use assistive devices, and communicate with your doctor. Most people don’t know that heat reduces stiffness, cold reduces swelling, or that a cane in the right hand actually takes pressure off the left knee.
The American College of Rheumatology says you need at least three of these four to see real results. Skipping one-especially exercise-makes the others less effective.
Medications: What Helps, What Doesn’t, and the Real Risks
Painkillers are common, but they’re not the solution. NSAIDs like ibuprofen or naproxen help with inflammation and pain short-term. But 32% of people stop taking them because of stomach issues, kidney strain, or high blood pressure. They don’t slow joint damage. They just mask the signal.
Topical creams with capsaicin or NSAIDs can be safer and just as effective for knee or hand OA. They don’t flood your system with chemicals.
Injections? Corticosteroids are the go-to for flare-ups. OARSI’s 2023 guidelines say they reduce knee pain by 50% for up to four weeks. They’re not a cure, but they can buy you time to get back into exercise. Hyaluronic acid injections? Evidence is mixed. Many patients report no benefit, and they cost hundreds per shot.
Now, there’s new hope: tanezumab, a nerve growth factor blocker approved by the FDA in June 2023. In trials, it cut pain 35% more than NSAIDs. But it’s reserved for moderate-to-severe cases because of rare side effects like joint damage. It’s not for everyone-but it’s proof that better options are coming.
What Doesn’t Work (and Why People Waste Money)
Glucosamine and chondroitin? Large studies, including one from the NIH in 2019, show they don’t reduce pain or slow joint loss any better than a placebo. They’re not harmful, but they’re not worth the $50 a month.
Stem cell and PRP (platelet-rich plasma) injections? They’re trendy, with over 380 active clinical trials worldwide. But right now, there’s no strong evidence they work better than saline injections. They cost $1,000-$3,000 per shot and aren’t covered by insurance. Wait for the science to catch up.
Braces? Unloader braces for knee OA can help if you have one-sided damage, but they’re bulky and uncomfortable. Most people stop using them after a few weeks.
And don’t fall for "miracle" supplements or magnetic therapy. No credible study backs them up. If it sounds too good to be true, it is.
When to Think About Surgery
Surgery isn’t failure-it’s the next step when everything else has been tried. Joint replacement (knee or hip) is one of the most successful surgeries in medicine. Over 90% of patients report major pain relief and improved mobility. Recovery takes months, but most people walk without pain within a year.
Doctors usually wait until:
- Pain is constant, even at rest
- Medications and therapy don’t help anymore
- You can’t do basic tasks like getting out of a chair or climbing stairs
- Your X-ray shows bone-on-bone contact (Grade 4 on the Kellgren-Lawrence scale)
There’s no rush. Many people wait too long and lose muscle, making recovery harder. Others rush in too early and regret it. Talk to your doctor. Get a second opinion. And make sure you’re physically ready-weight loss and strength training before surgery improve outcomes dramatically.

Real People, Real Results
On Reddit, a user named "KneePainSince40" wrote: "My knee OA started with occasional stiffness. After 10 minutes of walking, I’d be done. I lost 18 pounds, started physical therapy, and now I walk 3 miles every morning. Pain meds? I haven’t taken one in 14 months." Another patient, 67, said: "I thought I’d never play with my grandkids again. After six weeks of PT and cutting out sugar, I can kneel to help them build Legos. I didn’t know that what I ate affected my joints." These aren’t outliers. They’re people who followed the science-not the hype.
The Future Is Early Detection
Right now, we diagnose OA when the damage is already visible on X-rays. But experts like Dr. Virginia Byers Kraus say we’re too late. New blood tests are being developed to detect early biomarkers-proteins released by damaged cartilage-years before symptoms appear. Dr. Marc Hochberg predicts we’ll have these tests in five years.
That means prevention. If you’re 50, overweight, and have a family history, you could get tested before your knee aches. You could change your diet, start strength training, and stop OA before it starts.
Until then, the best tool you have is movement, weight control, and education. Not magic. Not pills. Just consistent, smart action.
Is osteoarthritis the same as rheumatoid arthritis?
No. Osteoarthritis is caused by mechanical wear and biological breakdown in the joint. Rheumatoid arthritis is an autoimmune disease where your immune system attacks your joints. OA pain gets worse with activity and improves with rest. RA pain is often worse in the morning and improves with movement. RA can affect other organs; OA doesn’t. Treatment is very different-RA needs immune-suppressing drugs; OA responds to exercise and weight loss.
Can osteoarthritis be reversed?
No, the damaged cartilage won’t grow back. But you can stop it from getting worse-and often improve how you feel. Studies show that losing weight, building muscle, and staying active can reduce pain, improve mobility, and delay the need for surgery. The joint structure may not heal, but your ability to function can improve dramatically.
Does cold weather make osteoarthritis worse?
Many people report more stiffness in cold or damp weather, but studies haven’t proven it causes more damage. The real issue is that people move less in winter, which makes joints stiffer. Keeping warm, staying active indoors, and using heat packs can help. It’s not the weather-it’s the inactivity.
What’s the best exercise for osteoarthritis?
The best exercise is the one you’ll do consistently. Low-impact cardio like walking, cycling, or swimming helps. Strength training for the muscles around the joint (quads, hamstrings, glutes) is critical. Tai Chi and yoga improve balance and reduce stiffness. Aim for 150 minutes a week-broken into 30-minute sessions five days a week. Even 10 minutes a day is better than nothing.
Should I use a cane or walker?
If you’re limping or leaning on furniture to walk, yes. A cane in the hand opposite your painful knee reduces pressure on the joint by up to 20%. A walker helps if you’re unsteady. They’re not signs of weakness-they’re tools that let you stay active longer. Get fitted by a physical therapist so you’re using it correctly.
Can diet affect osteoarthritis?
Yes, indirectly. No food cures OA, but losing weight through diet reduces joint stress. Anti-inflammatory foods-like fatty fish, berries, nuts, and leafy greens-may help reduce overall body inflammation. Avoiding sugary drinks and processed foods helps control weight and lowers inflammation. It’s not about a magic diet-it’s about eating to support your body, not fight it.
Next Steps: What to Do Today
If you have OA, start here:
- Track your pain for a week-when it happens, what makes it better or worse.
- Walk 10 minutes a day, three times this week. No need to push hard.
- Check your weight. If you’re overweight, aim to lose 5% in the next three months.
- Call your doctor and ask: "Can you refer me to a physical therapist who specializes in arthritis?"
- Visit the Arthritis Foundation’s website. Their free self-management course is evidence-based and easy to follow.
You don’t need to fix everything at once. One small step, repeated, changes everything.





3 Comments
I was skeptical about exercise at first but after 6 months of water aerobics and walking my knees don't scream anymore. It's not magic it's just moving
still take ibuprofen sometimes but way less now
You people act like losing weight is some profound revelation. Everyone knows fat kills your joints. The real problem is society lets you stay lazy and then sells you snake oil to feel better. Stop being victims and move your damn body
I love how this post breaks it down without shaming. My mom tried glucosamine for years then finally did PT and lost 12 lbs. She can now garden again and it's the best thing I've seen. No hype just real stuff that works