Penicillin-Cephalosporin Cross-Reactivity Calculator
Assess Your Risk
This tool helps determine the likelihood of reaction when considering cephalosporin antibiotics based on your penicillin allergy history. Remember: This is for educational purposes only and should not replace medical evaluation by a qualified allergist.
Results
More than 10% of people in the U.S. say they’re allergic to penicillin. But here’s the truth: 95% of them aren’t. That’s not a typo. Most of those labels were given after a childhood rash, a stomach upset, or a vague reaction years ago-none of which were true allergies. And yet, that label sticks. It changes everything-what antibiotics you get, how long you stay in the hospital, even your risk of deadly infections.
What Exactly Is a Beta-Lactam Allergy?
Beta-lactam antibiotics include penicillins (like amoxicillin and ampicillin) and cephalosporins (like ceftriaxone and cephalexin). They all share a core structure called the beta-lactam ring. That’s the part your immune system might mistake for a threat. But not all reactions are allergies. Many are side effects: nausea, diarrhea, or a mild rash from a virus you had at the same time. The real danger comes when a true IgE-mediated allergy is missed-or worse, when a false label leads doctors to avoid the safest, most effective drug.True penicillin allergy means your body makes IgE antibodies that trigger a rapid reaction: hives, swelling, wheezing, or even anaphylaxis within minutes to an hour. That’s rare-only 0.01% to 0.05% of penicillin courses cause anaphylaxis. But the fear? That’s everywhere.
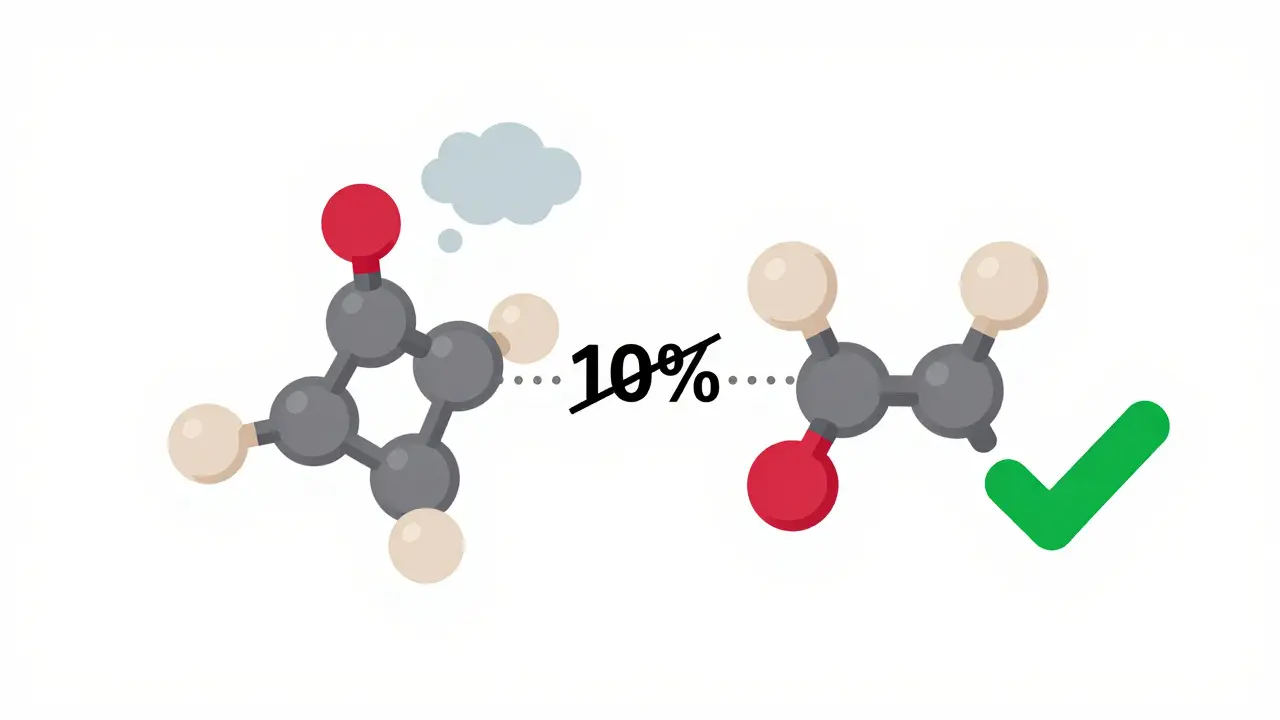
Penicillin vs Cephalosporin: The Real Risk of Cross-Reactivity
For decades, doctors were taught that if you’re allergic to penicillin, you can’t take cephalosporins. The old rule said 10% to 30% cross-reactivity. That’s what most medical charts still say. But that number is outdated.Modern studies show the real risk is closer to 1% to 3%-and only for first-generation cephalosporins like cephalexin. For later generations like ceftriaxone or cefdinir, the risk is practically zero. Why? Because their side chains-the parts that stick out from the beta-lactam ring-are completely different from penicillin’s. Your immune system doesn’t recognize them as the same threat.
Here’s the kicker: if you’ve never had a severe reaction to penicillin-no anaphylaxis, no swelling, no trouble breathing-you’re extremely unlikely to react to a cephalosporin. Yet, hospitals still avoid them. Why? Because of fear, not science.
What Do True Reactions Look Like?
A true penicillin allergy shows up fast. Within an hour, you might see:- Hives (red, itchy welts)-happens in 90% of cases
- Swelling of lips, tongue, or throat-seen in about half
- Wheezing, tight chest, trouble breathing-30% of cases
- Drop in blood pressure, dizziness, loss of consciousness-signs of anaphylaxis
These aren’t just uncomfortable. They’re life-threatening. But most people labeled “penicillin allergic” never had any of this. They got a rash after having mono. Or their skin itched after taking amoxicillin for an ear infection-and the doctor didn’t know it was likely viral. That’s not an allergy. That’s a coincidence.
Cephalosporin reactions follow the same pattern, but they’re rarer. The symptoms are identical, but the frequency is lower. And unlike penicillin, there’s no widely available skin test for cephalosporins. That makes diagnosis harder. But it doesn’t mean you can’t safely take them.
How Do You Know If You’re Really Allergic?
The only way to find out is testing. And it’s not complicated.If you think you’re allergic to penicillin, see an allergist. The gold standard is skin testing: two small pricks with penicillin derivatives, followed by an intradermal test if the first is negative. If both are negative, you’re almost certainly not allergic. The test’s negative predictive value? 97% to 99%. That means if it says you’re not allergic, you’re not.
For people with low-risk histories-like a mild rash that happened more than a year ago-doctors may skip the skin test and just give you a full dose of amoxicillin under observation. It’s called an oral challenge. Over 95% of people who’ve been labeled allergic pass it without a problem.
And here’s what most people don’t know: if you were labeled allergic 10 years ago, there’s an 80% chance you’ve outgrown it. Your immune system forgets. That’s why retesting is so important.
What Happens If You’re Still Labeled Allergic?
The consequences are serious-and expensive.Hospitals give you alternatives: vancomycin, clindamycin, fluoroquinolones. These drugs are broader, stronger, and more toxic. They wipe out good bacteria. That’s why patients with fake penicillin allergies are 30% more likely to get a Clostridioides difficile infection-a nasty, sometimes deadly gut bug. They’re also more likely to get surgical site infections because doctors can’t use the best antibiotic for the job.
And the cost? The CDC says it adds $2,000 to $4,000 per patient every year in extra drugs, longer hospital stays, and avoidable complications. That’s not just a medical problem. It’s a financial one.
One study found hospitals with formal penicillin delabeling programs cut broad-spectrum antibiotic use by 23% and reduced C. diff infections by 17%. That’s not a small win. That’s life-saving.
When You Really Need Penicillin-Desensitization
Some conditions only respond to penicillin. Think syphilis in pregnancy, neurosyphilis, or certain heart valve infections. If you’re labeled allergic but need penicillin, there’s a solution: desensitization.This isn’t a cure. It’s a temporary reset. You’re given tiny, increasing doses of penicillin every 15 to 30 minutes over 4 to 8 hours, under strict monitoring. Your immune system gets used to it. You can then complete your full course safely.
Success rates? Over 80%. But it’s not something you do at home. It requires a hospital, an allergist, and emergency equipment on standby. The CDC says this should only be done by trained specialists. And yes, the effect wears off. If you need penicillin again later, you’ll need to go through it again.

Why This Matters More Than You Think
This isn’t just about one drug. It’s about how we treat patients. We’ve created a system where a vague childhood reaction dictates adult care for decades. We avoid the safest, cheapest, most effective antibiotics because of outdated myths.And it’s getting worse. Only 35% of U.S. hospitals have formal programs to re-evaluate penicillin allergy labels. Rural hospitals? Only 28% have access to allergists. That means millions of people are stuck with labels that aren’t accurate-and the consequences are real.
But change is happening. Mayo Clinic’s delabeling program removed false allergy labels from 65% of eligible patients. Hospitals are starting to ask: “When exactly did this happen? What were the symptoms? Was it anaphylaxis?” They’re moving away from blanket labels and toward real data.
What Should You Do?
If you’ve been told you’re allergic to penicillin:- Don’t assume it’s true. Ask: “What happened? Was it a rash? Did I have trouble breathing?”
- If you’ve never had a severe reaction, ask your doctor about testing.
- If you need antibiotics for an infection and were denied penicillin or cephalosporins, ask why.
- If you’re pregnant and allergic to penicillin, get tested-syphilis treatment requires penicillin, and alternatives are riskier.
- Update your medical records. Don’t just say “penicillin allergy.” Say “rash at age 6, no breathing issues.” Specificity saves lives.
And if you’re a clinician? Stop using the old 10% cross-reactivity rule. Look at the generation of cephalosporin. Check the reaction history. Offer testing. You’re not just prescribing a drug-you’re choosing a treatment path that affects survival, cost, and long-term health.
What’s Next?
Researchers are working on faster, cheaper tests. A 2023 study identified two immune markers-IL-4 and IL-13-that could predict penicillin allergy with high accuracy. A $12.5 million NIH study is testing streamlined testing in community clinics, with results due in 2026.The goal? Make testing as easy as a blood draw. No more waiting weeks for an allergist appointment. No more avoiding life-saving antibiotics because of a label that doesn’t fit.
This isn’t about fear. It’s about facts. And the facts say: most penicillin allergies aren’t real. Most cephalosporin fears are overblown. And correcting this one mistake could change how millions of people are treated.



12 Comments
Been labeled penicillin-allergic since I was 5 after a rash from amoxicillin. Turned out it was mono. Got tested last year-zero reaction. Now I take amoxicillin like it’s candy. Why do we still treat these labels like holy scripture?
It’s fascinating-how a single, misinterpreted symptom from childhood can dictate medical decisions for decades… and yet, we don’t question it. We don’t re-evaluate. We don’t update. We just… keep going. The system’s built on inertia, not evidence. And that’s terrifying.
bro why is everyone so obsessed with penicillin like its the holy grail of antibiotics?? i mean cmon. we got like 50 other drugs. just take cipro or whatever. its fine. stop overthinking.
I had a cousin who was told she was allergic to penicillin after a rash at age 4. She spent 15 years on clindamycin for every infection. Then she got sepsis from a UTI-because the alternatives didn’t cover the right bugs. She finally got tested at 29. Turns out she’s fine. Now she’s a nurse. She tells every patient to ask: ‘Was it anaphylaxis?’ If not… maybe it’s not real.
It’s not just about antibiotics. It’s about how we listen-or don’t-to our patients’ histories.
So what you're saying is doctors are dumb and everyone's lying about allergies??
cool story bro
also i'm allergic to everything so whatever
I work in ER. We had a guy come in with pneumonia. Labelled penicillin allergic. We gave him azithromycin. He got C. diff. Spent 3 weeks in the hospital. Cost $28k. He had a mild rash at 8. No swelling. No breathing issues. We tested him after. Negative. He’s fine now. But his chart still says ‘allergic.’ Why? Because no one bothered to fix it. We’re all complicit.
If you’ve ever been told you’re allergic to penicillin and never had a real reaction-go get tested. Seriously. Do it. It’s 20 minutes. It could save your life. Or at least save you from being stuck with drugs that make you throw up for a week. Stop letting a childhood mistake control your adult health.
One must consider the possibility that this entire narrative is orchestrated by Big Pharma to push more expensive antibiotics upon the populace. The 95% statistic? Suspiciously convenient. Who funds these studies? Who profits when we avoid penicillin? The system is not designed to heal-it is designed to monetize.
Can we just admit that Americans are terrible at medicine? We label everything ‘allergy’ like it’s a TikTok trend. In Canada, we don’t do this. We test. We verify. We don’t let a 7-year-old’s rash haunt someone until they’re 70. This is why your healthcare costs are insane.
The immunological paradigm is fundamentally flawed when applied to non-IgE-mediated adverse drug reactions. The conflation of pharmacological side effects with true hypersensitivity constitutes a diagnostic fallacy of catastrophic proportions. The current clinical framework lacks epistemic rigor, and the persistence of outdated cross-reactivity heuristics reflects a pathological adherence to heuristic bias.
I’m a nurse practitioner in a rural clinic. We started a penicillin delabeling program last year. We used the oral challenge for low-risk patients. Out of 42 people we tested, 40 passed. One had a mild rash-turned out it was a virus. One had a true allergy. We’ve changed 40 lives. No more vancomycin. No more C. diff. No more $3,000 bills. It’s not magic. It’s just asking the right questions.
If you’re reading this and you’re labeled allergic-don’t wait. Ask your doctor. Bring this article. You deserve better.
It is imperative to note that while the prevalence of true penicillin allergy is indeed low, the clinical decision-making process must remain cautious, as anaphylactic reactions, though rare, carry a mortality rate of approximately 1% even with prompt intervention. Therefore, while delabeling is encouraged, it must be conducted under the supervision of a board-certified allergist with access to emergency resuscitation equipment, as per the 2022 AAAAI guidelines.