GLP-1 Weight Loss Calculator
How This Calculator Works
Based on clinical trial data from the article: Wegovy shows 15% weight loss (STEP-1 trial), Mounjaro shows 20% weight loss in non-diabetes patients, and Ozempic typically shows 10-15% loss. These are estimates - individual results vary significantly.
Your Estimated Weight Loss
Percentage of weight loss
Pounds lost
For years, people struggling with weight loss saw diabetes medications as something that had nothing to do with them. But that changed. Today, drugs like Ozempic, Wegovy, and Mounjaro are being used far more often for weight loss than for diabetes. And it’s not just a side effect-it’s the main reason millions are taking them.
How GLP-1 Agonists Actually Work
These drugs aren’t magic pills. They mimic a natural hormone in your body called GLP-1, which your gut releases after eating. This hormone tells your pancreas to make insulin when blood sugar rises-but it also sends signals to your brain that you’re full. That’s why people on these drugs feel less hungry, snack less, and stop eating sooner. The effects go deeper. GLP-1 agonists slow down how fast food leaves your stomach. That means you feel full longer. They also reduce cravings, especially for high-fat, high-sugar foods. In clinical trials, people didn’t just lose weight-they lost the urge to overeat. One user on Reddit described it as "my brain finally stopped screaming for snacks."Weight Loss Numbers That Matter
The results aren’t subtle. In the STEP-1 trial, people using semaglutide (Wegovy) lost nearly 15% of their body weight over 68 weeks-compared to just 2.4% with placebo. That’s like losing 30 pounds if you weigh 200. Tirzepatide (Mounjaro, Zepbound) did even better: 20% weight loss in people without diabetes, and over 11% in those with type 2 diabetes. These aren’t temporary drops. In studies lasting two years, most people kept the weight off as long as they stayed on the drug. But stop taking it? About half to 70% of the weight comes back within a year. That’s why doctors say these aren’t short-term fixes-they’re long-term tools.Beyond the Scale: Heart, Brain, and Liver Benefits
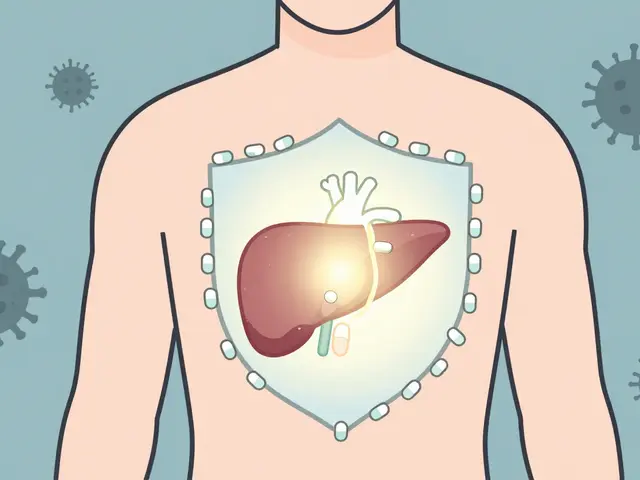
The real surprise? These drugs do more than shrink your waistline. People taking them have lower blood pressure, better cholesterol, and fewer heart attacks. A 2024 study from the University of Chicago found GLP-1 agonists cut the risk of major heart events by up to 18% and lowered overall death risk by 14% in people with heart disease risk factors. Even more unexpected: neurological benefits. A study of over 2 million veterans showed users had 23% fewer seizures, 17% lower risk of substance use disorders, and 14% less suicidal thinking. Researchers are now testing these drugs for Alzheimer’s and Parkinson’s, because GLP-1 receptors are found in the brain-and they seem to protect nerve cells. Liver fat? It drops too. Non-alcoholic fatty liver disease (NAFLD) improves significantly in users, even without major diet changes. That’s huge-NAFLD affects nearly 1 in 3 adults in the U.S. and can lead to cirrhosis if ignored.Who Benefits Most-and Who Doesn’t
These drugs work best for people with obesity (BMI 30+) or overweight with weight-related health issues like prediabetes, high blood pressure, or sleep apnea. They’re especially powerful for those with type 2 diabetes who’ve struggled with weight gain from insulin or other pills. But they’re not for everyone. Lean people without metabolic problems often see little benefit-and may still get side effects. The same goes for people with a history of pancreatitis, thyroid cancer, or multiple endocrine neoplasia. Doctors screen carefully before prescribing.Side Effects: Nausea, Vomiting, and the "Ozempic Face"
No drug is without trade-offs. About 30-50% of users get nausea, vomiting, or diarrhea, especially when starting. Most get used to it after a few weeks. But for some, it’s bad enough to quit. Then there’s "Ozempic face." Long-term users report a loss of facial fat-cheeks hollowing out, jawlines sharpening, skin looking looser. It’s not officially recognized by the FDA, but dermatologists and plastic surgeons are seeing it more often. Harvard Health reported it in 42% of users after a year or more. It’s not dangerous, but it can be startling.Cost and Access: The Biggest Hurdle
Wegovy costs about $1,349 a month without insurance. That’s more than most people can pay out of pocket. Insurance often blocks coverage unless you have diabetes or a BMI over 35 with a related condition. Even then, prior authorizations can take weeks. In 2024, 58% of users reported insurance issues. Some cut their dose in half to stretch the supply. Others stop entirely. Novo Nordisk offers a patient assistance program that covers 75% of costs for eligible people, but you have to apply-and not everyone qualifies.How to Use Them Safely
Doctors start low-0.25 mg of semaglutide once a week-and slowly increase over 16 to 20 weeks. This helps your body adjust and cuts down on nausea. Never rush the dose. More isn’t always better. Pair the drug with real lifestyle changes: protein-rich meals, regular movement, sleep hygiene. The weight loss sticks better when you’re not just relying on the pill. Telehealth programs like Found and Calibrate bundle medication with coaching, but cost $99-$149/month on top of the drug.




11 Comments
I tried Ozempic for 3 months. Lost 22 lbs. Nausea was brutal at first, but after week 4? Gone. My snacks? Just... gone. 🤯
The clinical data is compelling, but the real-world implications deserve deeper scrutiny. The mechanism of GLP-1 agonism-enhancing satiety via central nervous system modulation and gastric emptying delay-is well-documented in peer-reviewed literature, yet long-term metabolic adaptation remains understudied. Moreover, the phenomenon colloquially termed 'Ozempic face' may reflect subcutaneous adipose tissue depletion beyond aesthetic concerns, potentially impacting dermal integrity and facial biomechanics. Longitudinal studies are imperative.
I’ve seen so many people jump on this bandwagon without understanding it’s not a cure-it’s a tool. One friend lost 50 pounds, felt amazing, then stopped cold turkey and gained it all back plus 10. It’s not about the pill. It’s about what you do when you’re off it. Please, if you’re thinking about this, get a coach. Not just a prescription.
Let’s be real: this isn’t medicine-it’s a luxury product for the privileged. People who can afford $1,300/month and have insurance that doesn’t fight them are the only ones benefiting. Meanwhile, low-income folks with diabetes and obesity are stuck eating processed food while billionaires get to ‘reset’ their metabolism. This isn’t progress-it’s healthcare capitalism at its ugliest.
The neurological benefits are perhaps the most underreported aspect. In the UK, we’re seeing GPs refer patients with treatment-resistant depression and anxiety for off-label GLP-1 use-especially those with metabolic syndrome. The reduction in suicidal ideation isn’t anecdotal; it’s statistically significant. This isn’t just weight loss. It’s mental health intervention disguised as an obesity drug.
I’m a nurse, and I’ve seen this play out. People come in crying because they’ve been told their weight is ‘their fault’ for 20 years. Then they get on these drugs, and for the first time, their body listens. It’s not magic-it’s biology. And yes, the face thing is weird, but if you’re alive, breathing, and no longer needing a CPAP machine, you’ll take the hollow cheeks.
I’m on it. It works. I don’t want to talk about it anymore.
I used to eat entire pizzas by myself on the couch at 2 a.m. I’d cry after. Then I started Mounjaro. Now? I drink tea. I go for walks. I don’t even think about pizza. It didn’t fix me-but it gave me space to finally fix myself. I’m not ‘cured.’ I’m just not drowning anymore.
The entire GLP-1 industry is a pharmacological Ponzi scheme. You think you're treating obesity, but you're just creating dependency on a class of drugs that only work if you're already privileged enough to afford them. Meanwhile, the real issue-ultra-processed food subsidies, food deserts, sedentary labor-is ignored. This is capitalism's answer to systemic failure: sell people a pill and call it innovation. #BiohackingElite
i was on ozempic for 6 mths and lost 18kg but i had a lot of diarrea and my stomach hurt a lot at the start. now i stopped and i got back all the weight. but i think the drug is good for people who are really struggling. just need to be carefull with side effects
Your point about systemic neglect is valid, but it risks conflating access inequity with therapeutic efficacy. The biological mechanism of GLP-1 agonism-enhancing satiety via hypothalamic POMC neuron activation and vagal afferent signaling-is pharmacologically distinct from socioeconomic determinants of health. While cost barriers are unjust, dismissing the drug’s physiological impact as merely a ‘luxury product’ undermines evidence-based medicine. The solution lies in policy reform, not therapeutic nihilism.