More than 10% of Americans carry a label saying they’re allergic to penicillin. But here’s the truth: over 95% of them aren’t actually allergic. That label-often from a childhood rash, a stomach upset, or a misdiagnosis decades ago-isn’t just outdated. It’s dangerous. It’s pushing doctors to prescribe stronger, costlier, and more harmful antibiotics. And it’s making infections harder to treat for everyone.
Why a False Allergy Label Matters More Than You Think
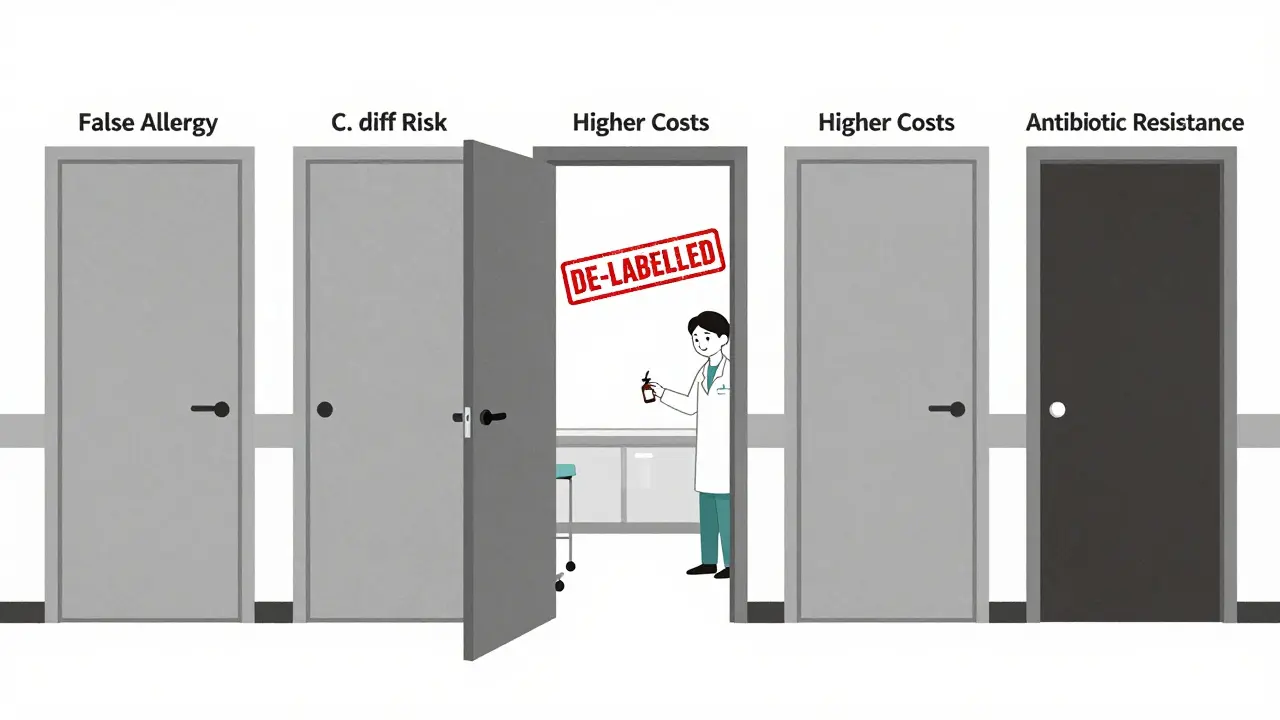
If you’ve been told you’re allergic to penicillin, you’ve probably been given alternatives like vancomycin, clindamycin, or fluoroquinolones. These drugs work, sure. But they’re not better. They’re broader-spectrum, meaning they wipe out good bacteria along with bad ones. That’s why patients with false penicillin allergy labels are 30% more likely to develop a C. diff infection-a severe, sometimes deadly gut infection caused by antibiotic overuse. The CDC estimates that false penicillin labels lead to 50,000 extra C. diff cases every year in the U.S. alone. That’s not a small number. It’s a public health crisis. And it’s not just about infections. Patients with these labels face higher hospital costs-about $1,000 more per person annually-because doctors are forced to use more expensive drugs. Hospitals pay more. Insurance companies pay more. You pay more in co-pays and lost work time. Worse, these alternative antibiotics are fueling antibiotic resistance. Patients with penicillin labels get clindamycin 69% more often and fluoroquinolones 28% more often than those without. That’s pushing bacteria like MRSA and ESBL-producing E. coli to evolve faster. These superbugs are already killing thousands each year. False allergy labels are helping them win.How Do You Know If Your Allergy Label Is Real?
Most people don’t remember how they got the label. Was it a rash after taking amoxicillin at age 7? A parent said it was an allergy. The doctor didn’t test it. The label stuck. That’s the story for nearly everyone with a penicillin allergy label. True IgE-mediated penicillin allergies-those that cause anaphylaxis, hives, or swelling-are rare. Only 1-2% of people who think they’re allergic actually have them. The rest? Their reactions were likely side effects: nausea, diarrhea, a mild rash that wasn’t allergic, or even a viral rash that happened to show up after taking the drug. The good news? We have a way to find out for sure. And it’s safe, fast, and accurate.The Testing Process: Skin Test, Then Challenge
The gold standard for confirming or removing a penicillin allergy label is a two-step process: skin testing followed by an oral challenge. Step 1: Skin TestingA tiny amount of penicillin (and its main breakdown products) is placed on your skin. A small prick or injection follows. If you’re truly allergic, your skin will react within minutes-redness, swelling, itching. But if nothing happens? That’s a strong sign you’re not allergic. Skin tests are over 95% accurate at ruling out IgE-mediated reactions. Step 2: Oral Drug Challenge
If the skin test is negative, you’re given a small dose of amoxicillin-usually 250 mg-under medical supervision. You wait 30 to 60 minutes. Then you get a full therapeutic dose. You’re watched for another hour. Less than 2% of people have any reaction at all. And almost all of those are mild: a little itching, a faint rash. No anaphylaxis. No hospital stays. This whole process takes about two hours. No needles beyond the skin test. No overnight stay. No risk of long-term harm. And the payoff? You can take the safest, most effective antibiotic for your next infection.

What If You Can’t Get to an Allergist?
You don’t need to see a specialist to start. Many primary care doctors, pharmacists, and even ER teams are now trained to do this safely. The PEN-FAST tool-a simple 5-question checklist-helps determine your risk level:- Was your reaction 5 or more years ago? (Yes = 1 point)
- Did you have anaphylaxis, angioedema, or wheezing? (No = 1 point)
- Did you need epinephrine or hospital care? (No = 1 point)
- Was your reaction a rash only? (Yes = 1 point)
- Are you now being treated for an infection? (Yes = 1 point)
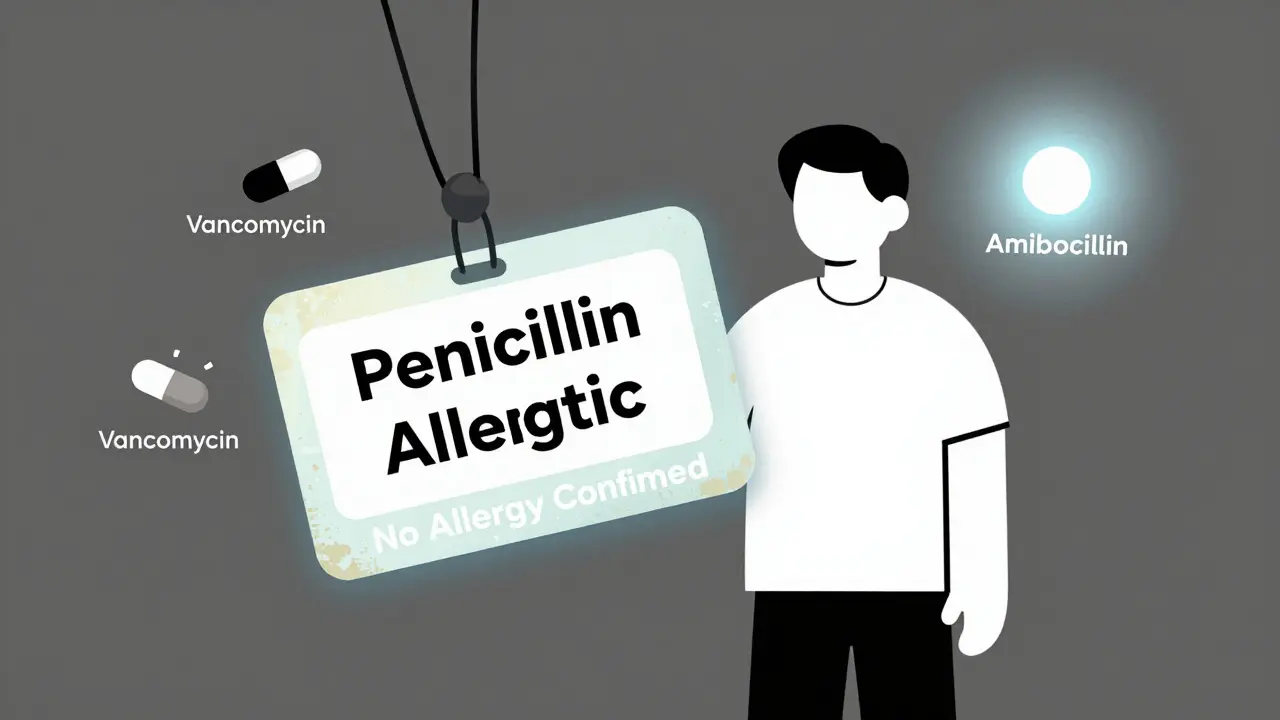
What Happens After You’re De-Labelled?
Once you’re cleared, your allergy status isn’t just erased. It’s updated with precision. You’re no longer labeled “allergic to penicillin.” You’re labeled “no penicillin allergy confirmed.” Sometimes, if you had a true reaction to a specific drug like amoxicillin, you’ll be told you’re allergic to that one drug only-not all penicillins. Your electronic health record gets updated. Your pharmacy gets notified. Your future doctors won’t avoid the best drug for your infection. You’ll get faster treatment. Fewer side effects. Lower bills. One 68-year-old patient in Massachusetts had a 40-year-old penicillin label. He kept getting complicated UTIs because doctors avoided amoxicillin. After testing, he was cleared. Within a year, he avoided two hospitalizations. His total healthcare costs dropped by $28,500 over two years.Why Isn’t Everyone Getting Tested?
The science is clear. The guidelines are solid. The tools exist. So why are only 12% of U.S. hospitals fully using de-labeling programs? Three big barriers:- Lack of access. There’s one allergist for every 500,000 people in rural areas. Waiting times for testing can hit 14 weeks.
- Patient fear. Many people are scared to try the drug again-even if they haven’t had a reaction in 30 years.
- System inertia. Hospitals don’t always update records. Pharmacists don’t always know how to flag de-labeled patients. EHR systems make it hard to change allergy status.
Real Stories: What Patients Say
On Reddit, a user named PenicillinCurious22 wrote: “I was told I was allergic since age 5. Got a rash. That was it. Did the test at Mayo Clinic-negative skin test, then two doses of amoxicillin. Now I take it for sinus infections. No stomach issues. No Z-Pak. Life’s easier.” Another person on HealthUnlocked had a bad experience: “They skipped the skin test and gave me the drug. I wheezed. Now I’m properly labeled as allergic. But I wish they’d tested first.” That’s the lesson: testing matters. Do it right. Don’t skip steps. Use the guidelines. And if you’re told you’re allergic-ask: “Was this tested? Or just assumed?”What You Can Do Today
If you’ve been told you’re allergic to penicillin-or any antibiotic-here’s what to do:- Check your medical records. What exactly was the reaction? When? Was it ever confirmed?
- Ask your doctor about the PEN-FAST score. Are you low risk?
- Request a referral to a drug allergy clinic or allergist. Many insurance plans cover this.
- If you’re in a hospital, ask if they have a penicillin de-labeling program.
- Don’t assume the label is accurate. Most aren’t.
It’s Not Just About You
Every time you get tested and cleared, you help everyone else too. Fewer broad-spectrum antibiotics used = less resistance. Fewer C. diff cases. Lower costs. Better outcomes. This isn’t just personal health. It’s public health. The data is overwhelming. The tools are ready. The time to act is now. Don’t let a 30-year-old mistake keep you from the best care possible.Can I be allergic to penicillin if I never had a reaction as an adult?
Yes, but it’s rare. Most penicillin allergies are diagnosed in childhood based on mild rashes or stomach upset, not true immune reactions. Studies show that 95% of people labeled allergic as kids outgrow it or were never allergic to begin with. The immune system changes over time. Testing is the only way to know for sure.
Is penicillin allergy testing safe?
Extremely safe when done properly. Skin testing has a near-zero risk of severe reaction. Oral challenges are done under supervision with emergency equipment on hand. Less than 2% of patients have any reaction at all, and nearly all are mild-like a slight rash or itching. Severe reactions are extremely rare. The risk of not testing-using worse antibiotics-is far higher.
Can I get tested if I’m not currently sick?
Yes, absolutely. In fact, it’s better to get tested when you’re healthy. Testing during an active infection can interfere with results. Most clinics schedule these tests as routine appointments. You don’t need to be sick to qualify.
What if the test shows I’m allergic?
If you have a true reaction during testing, you’ll be properly labeled for that specific drug (e.g., amoxicillin, not all penicillins). You’ll get a medical alert card and your records will be updated. You’ll still have treatment options-just not that one drug. Many people who test positive still have many safe antibiotic choices.
Will my insurance cover the test?
Most insurance plans, including Medicare and Medicaid, cover allergy testing when ordered by a doctor for confirmed suspicion of drug allergy. Many hospitals now offer the test as part of routine care with no extra charge. Ask your provider or hospital billing department-they can confirm coverage before you schedule.
How long does the whole process take?
Typically, the full process takes 2 to 3 hours. Skin testing takes about 30 minutes to set up and read. The oral challenge is done in two doses with 30-60 minutes between each, followed by a 60-minute observation period. You can usually go home the same day. Some clinics offer same-day results.
Can I be tested for allergies to other antibiotics too?
Yes. While penicillin is the most common, testing is also available for other beta-lactams like cephalosporins and carbapenems. Testing for non-beta-lactam antibiotics (like sulfa drugs or vancomycin) is less standardized but possible in specialized centers. Always ask if your specific drug can be tested.


3 Comments
This is one of those topics that should be taught in high school biology-seriously. Over 95% of people with penicillin labels aren’t allergic? That’s not just a statistic; it’s a systemic failure of medical documentation. I had my label removed last year after a 25-year-old rash from amoxicillin. The whole process took two hours. I didn’t die. I didn’t even get a rash. Now I take amoxicillin for every sinus infection, and my doctor doesn’t have to prescribe me $300 antibiotics anymore. Why isn’t this routine?
It is interesting how cultural perceptions of medicine shape our understanding of allergies. In many parts of India, the concept of 'drug allergy' is often conflated with side effects or even superstition. A child gets a rash, and the family assumes it's the medicine-no testing, no follow-up. The label sticks. But the real tragedy is not just the mislabeling-it's the lack of access to even basic allergy diagnostics in rural areas. The science exists, but the infrastructure does not. Until we bridge that gap, the problem will persist in silence.
bro this is wild. i was told i was allergic to penicillin when i was 6 because i got a rash after taking some syrup. never got tested. 20 years later, i had a bad UTI and my doc gave me cipro because ‘you’re allergic’. i ended up with a yeast infection and a $900 bill. just got tested last month-negative. took amoxicillin last week. no probs. why do docs just assume? it’s lazy. fix the system, not just the patient.