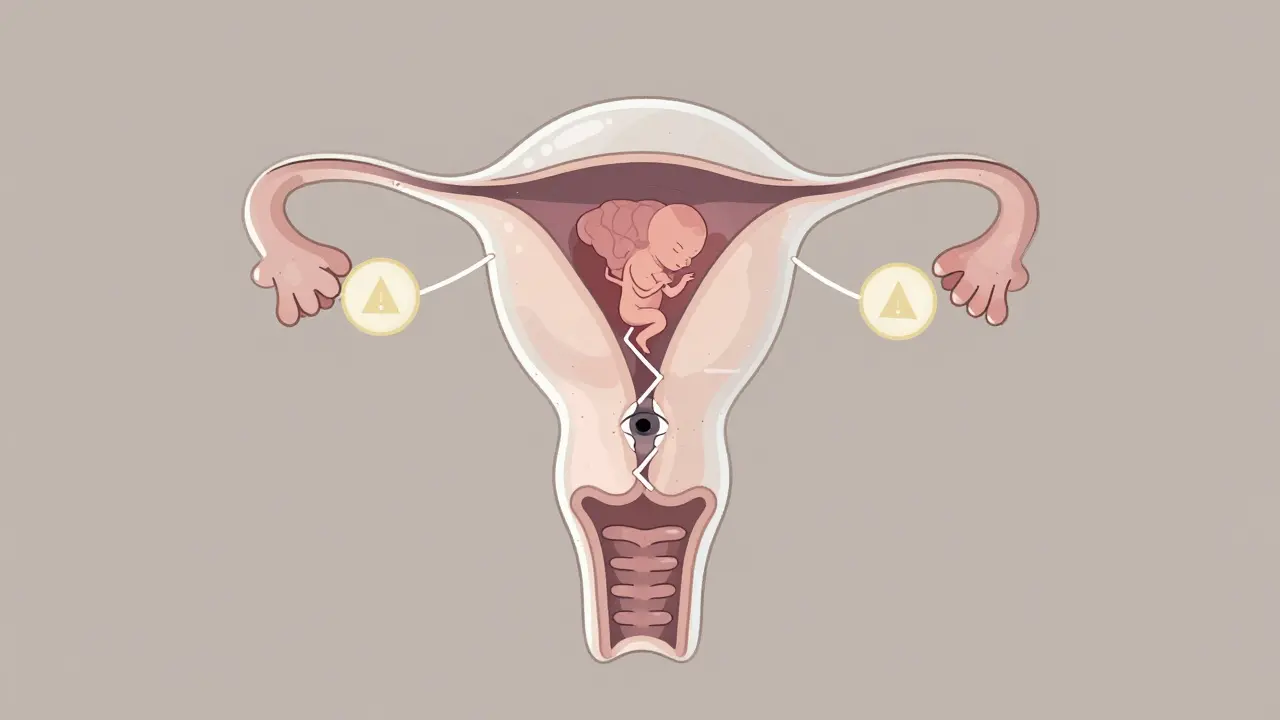
When you're pregnant and struggling with severe anxiety or insomnia, the pressure to find relief can feel overwhelming. Many women turn to benzodiazepines-medications like lorazepam, alprazolam, and diazepam-because they work quickly and effectively. But what happens when those pills cross the placenta? The answer isn’t simple, and it’s not something you can ignore.
What Are Benzodiazepines, and Why Are They Used in Pregnancy?
Benzodiazepines are a class of drugs developed in the 1950s to calm the nervous system. They’re prescribed for anxiety, panic attacks, muscle spasms, and sleep disorders. During pregnancy, about 1.7% of women in the U.S. get a prescription for one of these drugs during the first trimester, according to a 2024 JAMA Psychiatry study. That number has been rising steadily over the last decade.
Why? Because untreated anxiety and insomnia don’t just make life harder-they can raise the risk of preterm birth, low birth weight, and even postpartum depression. For some women, the stress of pregnancy itself triggers or worsens mental health symptoms. So doctors sometimes prescribe benzodiazepines as a last resort when therapy and lifestyle changes haven’t worked.
But here’s the catch: these drugs don’t stay in the mother’s bloodstream. They cross the placenta easily and build up in fetal tissue. That’s why experts are worried.
What Birth Defects Are Linked to Benzodiazepines?
The data is mixed, but several large studies point to real, if small, increases in certain birth defects. The most consistent findings come from two major sources: the CDC’s National Birth Defects Prevention Study and a 2022 nationwide cohort study in South Korea involving over 3 million pregnancies.
Here’s what the evidence shows:
- Dandy-Walker malformation: A rare brain defect affecting the cerebellum. Risk increased nearly 3 times with benzodiazepine exposure.
- Anophthalmia or microphthalmia (missing or underdeveloped eyes): This was strongly linked to alprazolam-the brand name Xanax. The risk jumped to 4 times higher in exposed pregnancies.
- Esophageal atresia or stenosis: A condition where the esophagus doesn’t form properly. Alprazolam was again the main driver, with a 2.7 times higher adjusted risk.
- Pulmonary valve stenosis: A heart defect where the valve leading to the lungs is narrowed. Lorazepam (Ativan) was tied to this in one study.
- Heart defects overall: A 14% increased risk was seen in the South Korean study, with higher daily doses (over 2.5 mg lorazepam-equivalent) showing stronger links.
These defects are rare. For example, Dandy-Walker malformation occurs in about 1 in 30,000 births. Even with a 3x increase, that’s still only about 3 in 30,000. But when you’re the parent, rarity doesn’t matter. One case is too many.
Is the Risk the Same for All Benzodiazepines?
No. Not all benzodiazepines carry the same risk. Alprazolam stands out in multiple studies as having the strongest association with eye and digestive tract defects. Lorazepam shows a clearer link to heart defects. Diazepam and clonazepam have less consistent data, but they’re not considered safe.
Why does this matter? Because if you’re on a benzodiazepine and pregnant-or planning to be-your doctor might be able to switch you to a different medication with a better safety profile. For example, some SSRIs (like sertraline) have more reassuring data for use in pregnancy than most benzodiazepines.
Don’t assume all these drugs are equal. The specific drug, the dose, and when you took it during pregnancy all change the risk picture.
What About Miscarriage, Preterm Birth, and Other Risks?
Beyond birth defects, benzodiazepines are linked to other serious outcomes:
- 85% higher risk of miscarriage after adjusting for other factors (JAMA Psychiatry, 2024)
- Increased risk of preterm birth and low birth weight
- Lower Apgar scores at 5 minutes-meaning the baby may struggle to breathe or adapt after birth
- Higher chance of NICU admission
- Higher risk of ectopic pregnancy even when taken just before conception
These aren’t just theoretical risks. In one study, for every 1,000 women who took benzodiazepines in the first trimester, about 8 more babies were born with major birth defects compared to those who didn’t. For heart defects, that number jumped to 14 extra cases per 1,000.
And here’s something important: the absolute risk is still low. Most babies born to mothers who took benzodiazepines are healthy. But when you’re making a decision about your pregnancy, even a small increase in risk can be too much.
What Do Experts Recommend?
Major medical groups agree: benzodiazepines should be avoided during pregnancy, especially in the first trimester.
- ACOG (American College of Obstetricians and Gynecologists): Recommends avoiding benzodiazepines in the first trimester unless absolutely necessary.
- APSA (American Psychiatric Association): Says treatment decisions must be individualized, with attention to drug type, dose, and timing.
- Canadian Guidelines: Say benzodiazepines should generally be avoided, but may be used in severe, treatment-resistant cases with close monitoring.
- FDA: Lists benzodiazepines as Pregnancy Category D-meaning there’s clear evidence of fetal risk.
- European Medicines Agency: Advises avoiding them in the first trimester unless the benefit clearly outweighs the risk.
These aren’t just cautious suggestions. They’re based on real data from millions of pregnancies. The bottom line? If you’re pregnant or trying to conceive, don’t start a benzodiazepine. If you’re already on one, don’t stop cold turkey-talk to your doctor.
What Are the Alternatives?
You don’t have to suffer through anxiety or insomnia alone. There are safer options:
- Cognitive Behavioral Therapy (CBT): Proven to work as well as medication for anxiety and insomnia during pregnancy. No side effects, no risk to the baby.
- Support groups: Talking to other pregnant women who’ve been through the same thing reduces isolation and stress.
- Exercise and sleep hygiene: Walking, yoga, and consistent bedtime routines can significantly improve sleep and reduce anxiety.
- SSRIs like sertraline: These antidepressants have the most safety data for pregnancy and are often the first-line choice for anxiety disorders.
- Non-benzodiazepine sleep aids: Melatonin (in low doses) and certain antihistamines like doxylamine (Unisom) are considered safer for short-term use.
Many women worry that therapy won’t work fast enough. But CBT doesn’t need to be a long-term commitment. Even 6-8 sessions can make a big difference.
What If You’re Already Taking Benzodiazepines?
If you’re pregnant and currently taking a benzodiazepine, here’s what to do:
- Don’t stop suddenly. Withdrawal can cause seizures, severe anxiety, and even harm the baby.
- Call your OB and psychiatrist together. They need to coordinate your care. One doctor can’t make this decision alone.
- Ask about tapering. A slow, controlled reduction over weeks is safer than quitting cold turkey.
- Explore non-drug options. Start CBT or another therapy now-even while you taper.
- Track your symptoms. Keep a journal of your anxiety, sleep, and mood. This helps your doctors adjust your plan.
Some women need to stay on medication because their anxiety is so severe it threatens their ability to care for themselves or their baby. In those rare cases, the lowest effective dose of the safest possible benzodiazepine (like lorazepam) may be used-with close monitoring.
What About Breastfeeding?
Benzodiazepines do pass into breast milk, but the amount is usually very small. However, some babies are more sensitive than others. Signs of exposure include excessive sleepiness, poor feeding, and trouble gaining weight.
If you’re breastfeeding and taking a benzodiazepine:
- Choose a short-acting drug like lorazepam over long-acting ones like diazepam.
- Take your dose right after nursing, not before.
- Watch your baby closely for drowsiness or feeding problems.
- Consider switching to non-benzodiazepine options if possible.
Most experts agree: breastfeeding while on a low dose of a short-acting benzodiazepine is usually safe-but it’s not risk-free. Talk to your pediatrician and your prescriber before making a decision.
Final Thoughts: It’s About Balance, Not Fear
No one wants to take a drug that could harm their baby. But no one wants to suffer in silence, either. The goal isn’t to scare you-it’s to give you the facts so you can make a choice that’s right for you and your baby.
For most women, the safest path is to avoid benzodiazepines during pregnancy. But if you’re already on one, or if your anxiety is so severe that you can’t function, you’re not alone-and you’re not failing. Help is available. Therapy, support, and safer medications exist. You don’t have to choose between your mental health and your baby’s safety. You can have both.
The key is to act early. Talk to your doctor before you get pregnant. If you’re already pregnant, don’t wait. Reach out today. You’re not alone in this.





12 Comments
Been on lorazepam for anxiety since college, now pregnant and terrified. Found this post after a 3am panic spiral. Glad I didn’t just quit cold turkey. Talking to my OB tomorrow about tapering and CBT. Thanks for laying out the risks without fearmongering.
THIS IS ALL BIG PHARMA LIES!! 😱 The CDC is funded by Pfizer!! My cousin took Xanax while pregnant and her kid is a genius who speaks 5 languages!! 🤯 They’re just trying to scare you so you’ll take their ‘safe’ SSRIs that make you numb!! 🚫💊 #FreeTheBenzos
Ugh. Another ‘Western medicine is evil’ article. In America we have the best doctors, the best science, and the best babies. If you’re Indian or somewhere with no healthcare, sure, maybe don’t take meds. But here? We’ve got resources. Why are you making moms feel guilty for using FDA-approved drugs? I’ve seen 100s of healthy babies born to moms on Ativan. This is just fear porn.
As someone who struggled with severe insomnia during both pregnancies, I get it. The guilt is real. But I switched to CBT + melatonin after week 8 and honestly? My sleep improved. No meds, no nightmares, just me and my baby sleeping through the night. You don’t have to choose between peace and safety-you can find both. 💪🌙
There’s a quiet tragedy in how we frame maternal health-as if the body is a battlefield between two lives. But it’s not. It’s one system, one organism, one story. The fear of harm becomes a kind of violence itself. Maybe the real question isn’t ‘is this drug safe?’ but ‘how do we support women so they never feel they need to choose?’
My sister took diazepam in her first trimester. Baby’s 7 now, plays piano, loves soccer, no issues. The stats are scary, but real life doesn’t always follow the curve. Context matters. Dose matters. Timing matters. Don’t let a study scare you into silence.
So… what if you’re already 12 weeks and you’ve been taking Xanax daily since week 4? Do you just… die? Is that the message? Because I’m not dying. I’m trying to survive. And now I’m supposed to feel like a monster?
According to the American College of Obstetricians and Gynecologists, the use of benzodiazepines during the first trimester is contraindicated unless the potential benefits clearly outweigh the risks. This is not a suggestion. It is a clinical guideline based on empirical data from over 3 million pregnancies. Please do not conflate anecdotal evidence with evidence-based medicine.
For anyone reading this and feeling alone-please know you’re not. I was on clonazepam during my pregnancy. I tapered slowly with my psych and OB. Started therapy. Joined a prenatal anxiety group. Now my daughter is two and thriving. It wasn’t perfect. But it was possible. And you deserve support, not shame.
wait so xanax causes eye defects?? but i took it for 3 months and my kid has perfect vision?? maybe its just bad luck??
It’s funny how we treat pregnancy like a chemical experiment. We worry about every pill, every bite, every breath-but never ask why the system fails women so badly that they feel forced to choose between mental survival and fetal safety. The real defect isn’t in the drug. It’s in the lack of accessible, non-pharmaceutical care.
I used to be a skeptic. Thought ‘therapy’ was just talking. Then I had a panic attack during my 16-week scan and couldn’t breathe. My OB referred me to a therapist who specialized in perinatal anxiety. Six sessions. Breathing techniques. Journaling. CBT didn’t ‘cure’ me-but it gave me back control. No meds. No guilt. Just me, my baby, and a little more peace. If you’re reading this and scared-reach out. Not to Reddit. To a human. You don’t have to do this alone.