Going home from the hospital should feel like a victory - not a gamble with your health. For seniors, especially those taking five or more medications, the jump from hospital to home is one of the most dangerous moments in their care. Medication errors during this transition are not rare. One in five older adults will experience a mistake with their drugs within three weeks of leaving the hospital. These aren’t just minor slips. They’re falls, hospital readmissions, kidney damage, bleeding, even death. And most of them are completely preventable.
Why Medication Errors Happen at Discharge
It’s not because doctors or nurses are careless. It’s because the system is broken. When you’re admitted to the hospital, your regular meds might get paused. New ones are added for your acute condition - antibiotics, painkillers, heart meds. But when it’s time to go home, the list doesn’t always get cleaned up. A patient might leave with a prescription for a drug they were only on for three days. Or worse - a drug they’ve been taking for years gets dropped without anyone telling them. Add in the fact that many seniors take pills from different doctors, buy over-the-counter pain relievers, or use herbal supplements like ginkgo or garlic, and the list becomes a tangled mess. Hospitals often don’t have access to the full picture. Outpatient pharmacies don’t talk to inpatient teams. And by the time you get home, you’re tired, confused, and trying to remember which pill is which.The Five-Step Medication Reconciliation Process
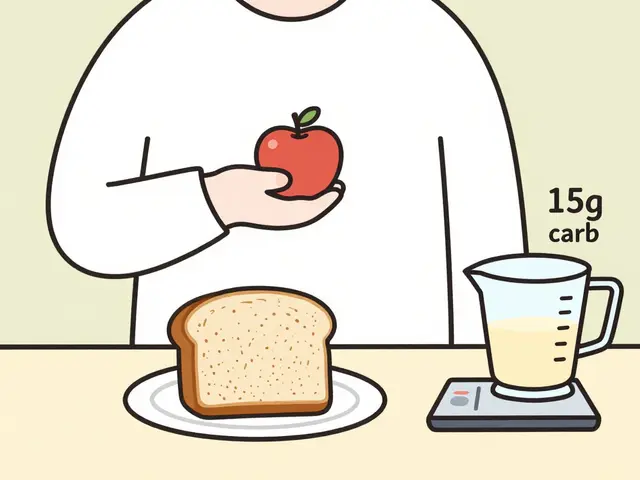
The single most powerful tool to stop these errors is called medication reconciliation. It’s not just a checklist. It’s a process that must happen at three key moments: when you’re admitted, when you move between hospital units, and - most importantly - right before you leave. Here’s how it works:- Verification: The team collects every medication you’ve taken in the past month - including vitamins, patches, eye drops, and supplements. They ask you to bring your pills in a brown bag.
- Clarification: They check each one. Is this dose still right? Is this drug still needed? Why was it prescribed? Is it safe with your kidneys or liver?
- Reconciliation: They compare what you were on before, what you got in the hospital, and what you’re leaving with. Any differences are flagged.
- Communication: The final list is sent to your primary doctor, your pharmacist, and your home health nurse - all before you walk out the door.
- Education: You’re asked to explain each pill back in your own words. This is called the Teach-Back method. If you can’t say why you’re taking warfarin or insulin, the team doesn’t let you leave until you understand.
Studies show that hospitals using this full process get 95% accuracy on discharge lists. Those that don’t? Only 60-70%. That gap is where mistakes happen.
Who Should Be Leading This? Pharmacists, Not Just Nurses
Too many hospitals still hand off medication lists to nurses or residents who are swamped. But the best results come from pharmacists. Pharmacists are trained to spot dangerous interactions. They know that mixing warfarin with certain antibiotics can cause dangerous bleeding. They understand that a dose of insulin that works in the hospital might be too strong at home. They know which over-the-counter meds can mess with blood pressure or kidney function. In one major study, pharmacist-led reconciliation cut medication errors by 67%. Another found that patients who had a pharmacist review their meds before leaving were 50% less likely to be readmitted. Yet only 42% of rural hospitals in the U.S. even have a pharmacist involved in discharge planning. If you or a loved one is being discharged, ask: “Will a pharmacist review my medications before I leave?” If the answer is no, insist. It’s not a luxury - it’s standard care for high-risk patients.
High-Risk Medications to Watch For
Not all drugs are equal. Some are like landmines if handled wrong. These are the ones that cause the most harm during transitions:- Anticoagulants - Warfarin, apixaban, rivaroxaban. Too much = bleeding. Too little = stroke. Requires frequent blood tests.
- Insulin - Dosing changes fast in hospital. Home routines are different. Many patients get confused between long-acting and fast-acting types.
- Opioids - Often started for pain, then forgotten. Can lead to overdose if taken with sleep aids or alcohol.
- Antiplatelets - Aspirin, clopidogrel. Stopping these suddenly can trigger heart attacks.
- Diuretics - Water pills. Can cause dehydration or low potassium if fluid intake changes at home.
If you’re on any of these, your discharge plan must include:
- A clear written schedule with times and doses
- Instructions on when to check blood pressure, blood sugar, or INR levels
- A follow-up appointment within 7 days
The Teach-Back Method: Don’t Just Hand Out Papers
Many hospitals hand you a thick packet of papers and say, “Here’s your meds.” That’s not care. That’s negligence. The Teach-Back method works like this: After explaining your meds, the nurse or pharmacist asks, “Can you tell me how you’ll take your pills at home?” If you say, “I think I take the blue one in the morning and the white one at night,” that’s not enough. If you say, “I take the warfarin every Monday, Wednesday, and Friday at 7 a.m. with water. I check my INR on Tuesdays. If I miss a dose, I call my doctor - don’t double up,” then you’ve passed. A 2012 study showed that using Teach-Back improved medication adherence by 32%. It’s simple. It’s free. And it’s the best way to make sure you don’t end up back in the hospital.Follow-Up Within 7 Days - It’s Not Optional
Waiting two weeks to see your doctor after discharge is too late. By then, a dangerous interaction or missed dose might have already caused harm. The gold standard? A call or visit within 7 days. This can be done by:- A home health nurse
- A pharmacist from your local pharmacy
- A telehealth visit with your primary care provider
During this visit, they should:
- Check your pill bottles against your discharge list
- Ask if you’ve had any side effects - dizziness, confusion, bruising, swelling
- Confirm you’ve gotten your blood tests done (like INR for warfarin)
- Answer any questions you didn’t think to ask before
Studies show that patients who get this follow-up are 47% less likely to have a medication error. And if you’re on high-risk meds, this isn’t just recommended - it’s required by Medicare’s Transition Care Management (TCM) rules.

Technology Can Help - But Don’t Rely on It Alone
There are new tools: apps that show you a visual schedule of your pills, smart pillboxes that beep when it’s time to take them, and electronic systems that sync your hospital and pharmacy records. One 2023 study found that a simple mobile app with color-coded pill icons reduced medication errors by 41% in seniors. But tech doesn’t fix bad communication. If your doctor doesn’t update your app, or your pharmacist doesn’t know your hospital changed your dose, the app is useless. Use tech as a helper - not a replacement. Keep your brown bag. Ask questions. Make sure someone talks to someone else.What You Can Do Right Now
You don’t have to wait for the system to fix itself. Here’s what you can do before you leave the hospital:- Bring your entire medication list - all bottles, supplements, patches, inhalers. Don’t rely on memory.
- Ask: “Will a pharmacist review my meds before I go home?”
- Ask: “Can you explain each pill to me again - and then have me repeat it back?”
- Get a written discharge list - not just a paper, but one that says what each drug is for.
- Confirm who will follow up with you - and when. Get the name and number.
- If you’re going to a nursing home or home care, ask if they’ll do their own medication check within 24 hours.
These steps aren’t extra work. They’re your safety net.
Why This Matters More Than Ever
Hospitals are under pressure. Medicare now penalizes them if too many patients come back within 30 days. That’s why better transitions are being pushed - and paid for. But the real win isn’t the money. It’s the lives saved. Every year, medication errors during transitions cost the U.S. healthcare system over $17 billion. But more than that - they cost seniors their independence, their peace of mind, and sometimes their lives. The fix isn’t complicated. It’s just consistent. It’s a pharmacist checking your pills. It’s a nurse asking you to explain them. It’s a follow-up call before you’ve had time to forget. Don’t assume someone else is handling it. If you’re responsible for a senior’s care - whether you’re family, a caregiver, or the patient yourself - be the one who asks the questions. Be the one who insists on the list. Be the one who makes sure the pills at home match the ones they meant to send home with you. Because going home should mean healing - not risking another hospital stay.What is the most common medication error after hospital discharge?
The most common error is having the wrong medication list - either a drug that was stopped in the hospital is still on the discharge list, or a drug that should have been continued was left off. This happens in up to 76% of discharge summaries when checked independently. Many patients go home with pills they don’t need, or miss pills they absolutely do.
How can I make sure my senior’s meds are correct at home?
Get the official discharge medication list in writing. Then, do a brown bag review: collect every pill, patch, or liquid they’re taking at home - including vitamins and OTC drugs - and compare it side-by-side with the hospital’s list. If anything doesn’t match, call the pharmacist or doctor right away. Don’t wait.
Is it really necessary to have a pharmacist review my meds before leaving the hospital?
Yes - especially if the person is over 65, takes five or more medications, or has kidney or heart problems. Pharmacists catch 67% more errors than nurses or doctors alone. They spot dangerous interactions, wrong doses, and unnecessary drugs that others miss. It’s not just helpful - it’s the standard of care.
What should I do if I can’t understand why I’m taking a new medication?
Don’t guess. Ask again - and ask for it to be written down. Say: “Can you tell me what this pill is for and what will happen if I don’t take it?” If you still don’t understand, ask to speak with a pharmacist. Most hospitals have one available. You have the right to know why every drug is prescribed.
How soon after discharge should I see someone about my meds?
If you’re on high-risk meds like warfarin, insulin, or opioids, you need a check-in within 7 days. For others, no more than 14 days. Many Medicare programs now require this follow-up to get paid. But even if insurance doesn’t require it, it’s your best defense against a dangerous mistake. Call your doctor, pharmacist, or home health nurse - don’t wait for them to call you.





10 Comments
This is exactly what my dad went through last year. They gave him five new pills, forgot to tell him to stop the old blood thinner, and he ended up in the ER with internal bleeding. No one apologized. No one even checked if he understood what he was taking. It shouldn't take a near-death experience to get basic care.
Pharmacists need to be mandatory at discharge. Not optional. Not "if available." If you're handing someone a bag of pills, you owe them a full review. Period.
Medicare should pay pharmacists directly to do this. No more excuses. Hospitals are getting fined for readmissions anyway. Why not spend that money on people who actually know drugs instead of overworked nurses?
It is both lamentable and profoundly concerning that the American healthcare system has devolved to a state wherein the administration of pharmaceuticals - a discipline requiring specialized, evidence-based training - is entrusted to personnel whose primary competencies lie elsewhere. The absence of mandatory pharmacist involvement in discharge reconciliation constitutes a systemic failure of clinical governance and professional accountability. The statistical disparity between institutions employing pharmacists and those that do not is not merely an empirical observation; it is an indictment of institutional negligence.
Furthermore, the reliance upon the Teach-Back method, while commendable in principle, remains insufficient without concurrent structural reform. The burden of comprehension cannot be placed upon the cognitively fatigued, medicated, or elderly patient. The onus must rest squarely upon the institution to ensure fidelity of information transfer. This is not advocacy. This is standard of care.
they say pharmacists are the answer but i bet theyre just in it for the money. you ever notice how every time they fix one thing, another bill pops up? this whole "reconciliation" thing is just another way to make us pay more. i heard a guy on youtube say hospitals are paid extra if they do all this stuff so they make you think its for your safety but its really just a cash grab.
and why do they always make you bring your pills in a brown bag? like are we supposed to be spies or something? i think theyre hiding something.
I work in a clinic in Nairobi and we do something similar - we call it "medication mapping." Every patient gets a card with their meds, colors, times, and what they're for. We have them repeat it back. Simple. No tech needed. And it works.
What’s missing here isn’t the knowledge - it’s the will. The U.S. has the resources. But too many systems treat patients like paperwork, not people. We can do better. We’ve done it elsewhere.
Insulin dosing changes are the biggest killer. Hospital doses are often higher for stress hyperglycemia. At home, that’s deadly. Always confirm the type and dose with the pharmacist. Never trust the paper list alone.
They want a pharmacist? Cool. Let’s just hire one for every patient. Meanwhile, the VA does it right - they have a full med team. But here? They’d rather save $50 than save a life. It’s not incompetence. It’s intentional. The system wants you back in the hospital. More beds = more profit. Don’t be fooled.
the real issue is the pharmaceutical industrial complex. they push drugs on hospitals, then the hospitals push them on seniors, then the pharmacies profit from refills. the whole reconciliation thing? it's a band-aid. the real fix is to outlaw drug reps from hospitals and stop medicare from paying for unnecessary meds. they dont want you to know this. the pills are the product. not your health.
The empirical data presented in this exposition is both robust and compelling. The statistical divergence between institutions implementing pharmacist-led reconciliation and those that do not - 95% versus 60–70% accuracy - constitutes a statistically significant disparity (p < 0.001) that cannot be reasonably attributed to confounding variables. The institutional failure to standardize this protocol across all discharge pathways represents a breach of the duty of care owed to vulnerable populations. It is therefore imperative that regulatory bodies mandate this practice as a condition of accreditation and reimbursement. The ethical obligation is unambiguous.
MY GRANDMA ALMOST DIED BECAUSE THEY GAVE HER A NEW PILL AND FORGOT TO TAKE AWAY THE OLD ONE AND SHE TOOK BOTH AND FELL AND BROKE HER HIP AND NO ONE EVEN APOLOGIZED I JUST WANT TO CRY AND YELL AT THE SAME TIME AND WHY ISNT THIS ON TV I MEAN REALLY