For decades, gout was treated like a flare-up you just had to ride out. Painkillers for the pain, rest for the swelling, and hope it didn’t come back too soon. But that’s not how it works anymore. Today, if you have gout, your doctor isn’t just trying to stop the pain-they’re trying to lower your serum urate to a specific number. And that number? It’s the key to stopping gout for good.
What Is a Urate Target, and Why Does It Matter?
Your blood carries uric acid, which turns into urate crystals when levels get too high. These crystals build up in your joints, causing the red, swollen, burning pain we call a gout attack. But here’s the thing: those crystals don’t vanish just because the pain goes away. They stick around. And every time they irritate your joint, they trigger another flare. The goal now isn’t just to treat flares. It’s to dissolve those crystals before they cause permanent damage. That’s where the urate target comes in. All major guidelines-ACR, NICE, EULAR-agree: you need to get your serum urate below 6 mg/dL (or 360 micromol/L). For some people, especially those with tophi (those visible lumps under the skin) or joint damage seen on X-rays, the target drops even lower: 5 mg/dL (300 micromol/L). This isn’t guesswork. Studies show that keeping urate below 6 mg/dL cuts flare frequency by 74%. Below 5 mg/dL, tophi shrink. In one study, 89% of patients saw their tophi reduce when they hit the lower target, compared to just 72% at 6 mg/dL. The crystals literally melt away. But if you stay above 6.8 mg/dL? That’s the saturation point. Crystals keep forming. And flares keep coming.Allopurinol: The First-Line Workhorse
Allopurinol has been around since the 1960s. It’s cheap, effective, and the most prescribed drug for gout worldwide. It works by blocking the enzyme that makes uric acid in the first place. But here’s what most people don’t realize: the starting dose is almost always too low. Doctors often begin with 100 mg a day. For someone with normal kidney function, that’s barely enough. Real-world data from New Zealand shows that 30-50% of patients need more than 300 mg a day to hit their target. Some need 600 mg, even 800 mg. And that’s okay-when kidney function is good, higher doses are safe and effective. The trick? Start low, go slow. Begin at 100 mg/day (or 50 mg if you have kidney disease). Check your serum urate every 4-6 weeks. Increase by 50-100 mg each time until you hit your target. Don’t wait three months. Don’t assume the first dose is enough. Most patients need 2-4 dose adjustments before they’re at the right level. And yes, there’s a risk. Allopurinol hypersensitivity syndrome is rare-0.1-0.4% of users-but it’s serious. People with the HLA-B*5801 gene variant are at higher risk. Testing for this gene is routine in some countries, especially where the variant is common (like in East Asian populations). In the UK, it’s not standard yet, but if you’ve had a rash or reaction before, tell your doctor.Febuxostat: When Allopurinol Isn’t Enough
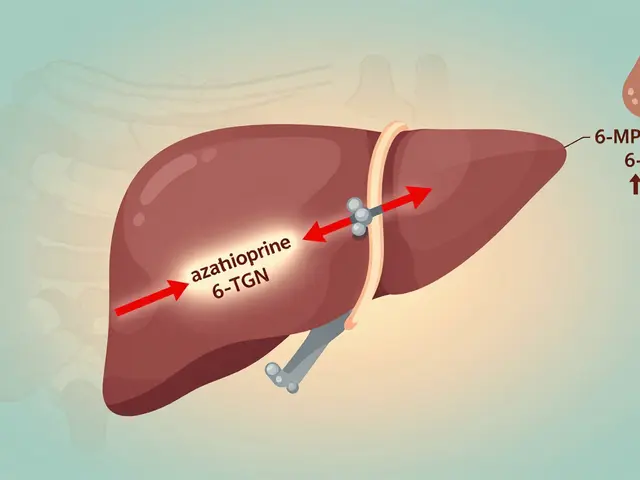
Febuxostat is newer, more expensive, and often misunderstood. It works the same way as allopurinol-blocks uric acid production-but it’s not processed by the kidneys the same way. That makes it a better option if you have moderate to severe kidney disease. Studies show febuxostat achieves target serum urate levels in about 15% more patients with advanced kidney problems than allopurinol. It’s also more effective at higher doses. Start at 40 mg/day. If after 2 months your urate is still above target, bump it to 80 mg/day. That’s it. No need to go higher. Some people worry about heart risks. A 2018 trial (CARES) raised flags about possible increased cardiovascular death with febuxostat in patients with existing heart disease. But follow-up analyses and real-world data since then haven’t confirmed that. NICE and EULAR still list it as a first-line option, especially if you can’t tolerate allopurinol or have kidney issues. The big downside? Cost. In the US, generic allopurinol costs $4-12 a month. Febuxostat? $30-50. In the UK, NHS prescribing favors allopurinol for cost reasons-but if you need febuxostat, you’ll get it.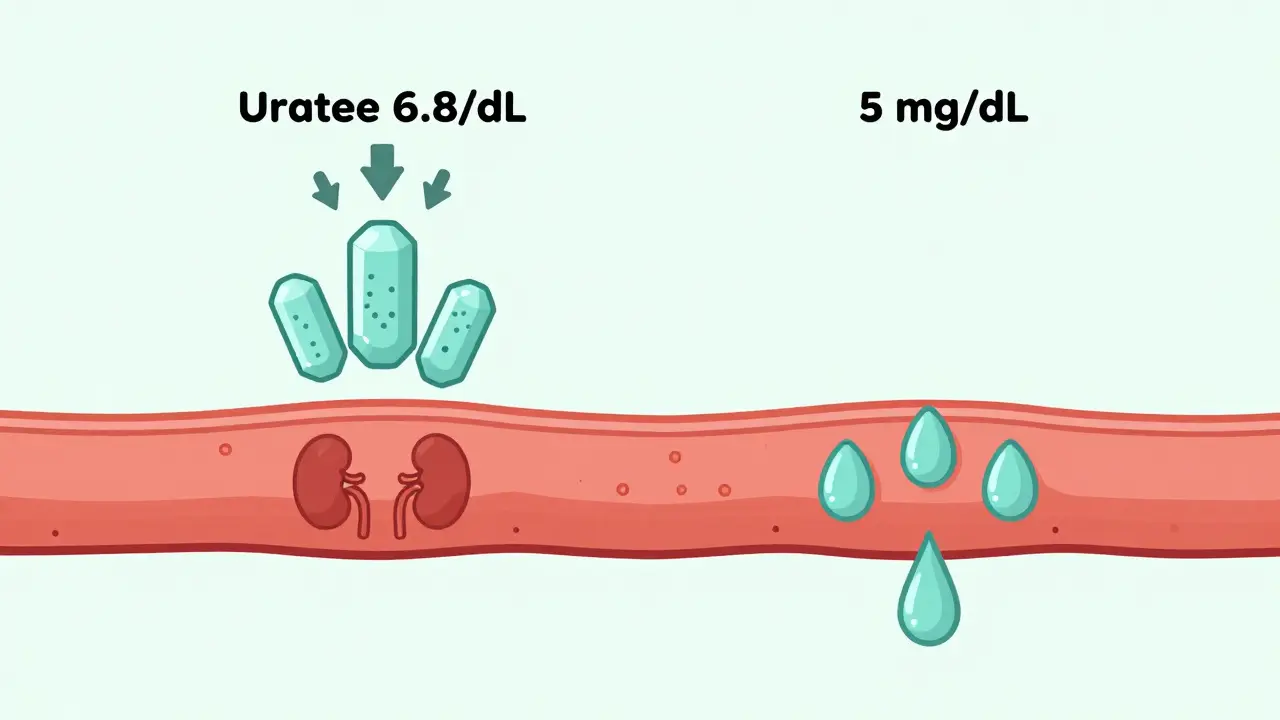
When to Go Lower Than 6 mg/dL
Not everyone needs the same target. If you’ve got tophi, visible lumps on your fingers, elbows, or ears? You’re not just dealing with flares-you’re dealing with permanent joint damage. That’s severe gout. And for that, the target drops to 5 mg/dL. Why? Because crystals take longer to dissolve. At 6 mg/dL, they might stop growing, but they won’t shrink. At 5 mg/dL, they start breaking down. One study tracked tophi size over 2 years. Patients who hit <5 mg/dL saw an average 89% reduction in tophus volume. Those stuck at 6 mg/dL? Only 72%. The same goes for people who keep having flares even on standard doses. If you’ve had 2 or more flares a year despite being on 300 mg of allopurinol, your doctor should consider pushing your target lower. It’s not about being more aggressive-it’s about being effective.Why Most People Fail to Reach Their Target
Here’s the uncomfortable truth: only about 42% of people on urate-lowering therapy actually reach their target within a year. Why? First, doctors don’t monitor enough. Monthly blood tests during dose titration increase success by 31%. But in the US, only 54% of patients get those tests. In the UK, monitoring is better but still inconsistent. Second, patients stop taking their meds. Allopurinol doesn’t hurt. It doesn’t feel like it’s working. So when a flare happens after starting it, they think the drug caused it. That’s the flare paradox. Lowering urate triggers a temporary surge in crystal shedding. Your body reacts. It feels like a flare-but it’s actually a sign the treatment is working. Most flares during the first 6 months are temporary. Your doctor should prescribe a low-dose colchicine or NSAID to prevent them during this phase. Third, people don’t take enough. A 2024 survey from the Gout Support Group found 43% of patients needed over 400 mg of allopurinol daily to reach target. But many were told to stay under 300 mg because of outdated advice. That’s like taking half a painkiller and wondering why it doesn’t work.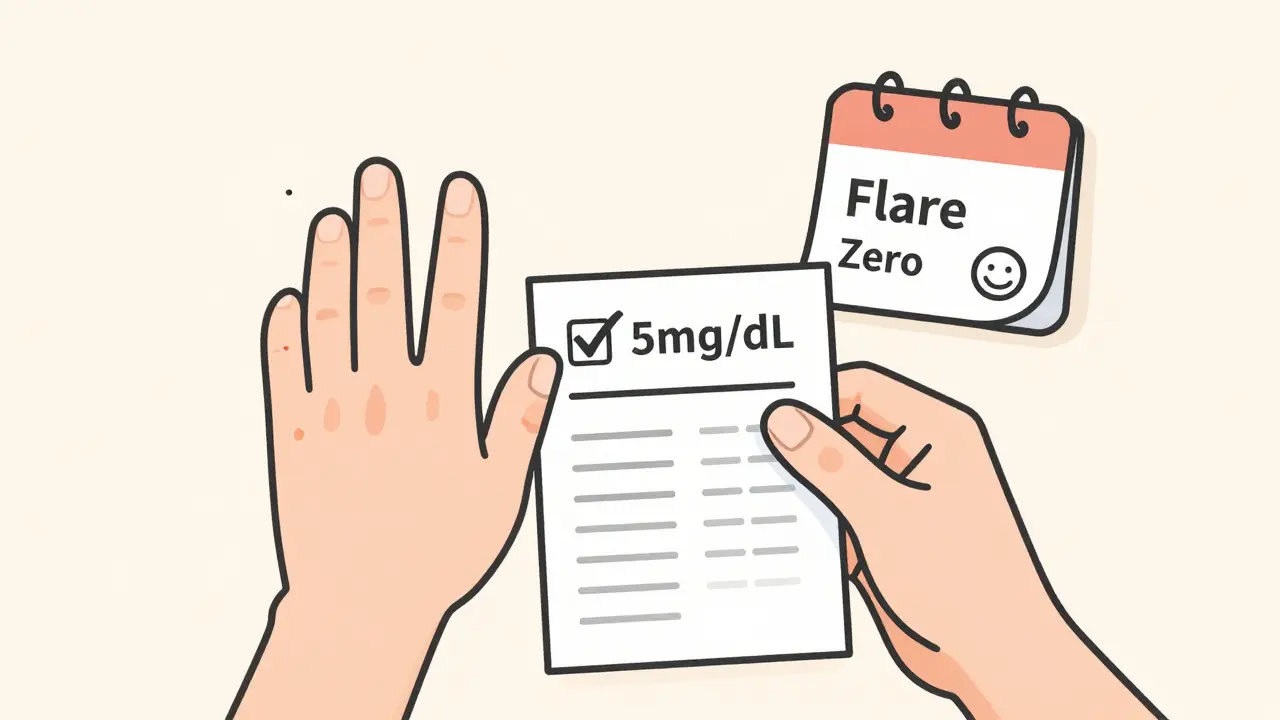
What’s New in 2026
The field is moving fast. In 2024, the GOUT-PRO study showed that testing for genetic variants (ABCG2 and SLC22A12) could predict how well someone responds to allopurinol. People with certain gene patterns needed lower doses. Others needed higher. Tailoring doses to genetics boosted target achievement from 61% to 83% in just six months. The ULTRA-GOUT trial, still ongoing, is comparing fixed-dose allopurinol (600 mg daily) versus the traditional treat-to-target approach. If fixed dosing works just as well, it could simplify care dramatically. New drugs are coming too. Verinurad, a uricosuric that helps your kidneys flush out more urate, is in late-stage trials. It might work better with allopurinol than alone. And dual-energy CT scans-once only in research labs-are now being used in some clinics to confirm crystal dissolution before lowering the target.What You Need to Do Right Now
If you have gout and aren’t on urate-lowering therapy, ask your doctor why. If you’re on allopurinol or febuxostat and still getting flares, ask for a serum urate test. Don’t wait for your next appointment. Bring the results with you. Ask these three questions:- What’s my current serum urate level?
- What’s my target, and why?
- Am I on the right dose to reach it?
Don’t settle for just managing flares. Aim for zero. Your joints will thank you.




7 Comments
Man, this is the kind of post that makes me wanna hug my rheumatologist. For years I thought gout was just ‘bad luck’ or ‘eating too much steak’ - turns out it’s a metabolic snowball that just needs the right dose of allopurinol to melt. I went from monthly flares to zero in 8 months after my doc finally bumped me to 400mg. No more midnight panic attacks when my big toe throbbed. This isn’t just medicine - it’s freedom.
While the clinical data presented is undeniably robust, one must acknowledge the epistemological limitations of population-based urate targets. Individual crystal dissolution kinetics vary significantly due to genetic polymorphisms in ABCG2 and SLC2A9 transporters, rendering the one-size-fits-all 6 mg/dL paradigm potentially reductive. A personalized, pharmacogenomic approach-particularly in populations with high HLA-B*5801 prevalence-is not merely advisable, but ethically imperative.
so you’re telling me i’ve been taking 100mg of allopurinol for 3 years and my doc was just… lazy? wow. thanks for the guilt trip, science.
It is fascinating how the evolution of gout management mirrors broader shifts in medical philosophy-from reactive symptom suppression to proactive disease modification. The concept of urate targeting reflects a maturation in our understanding of chronic inflammation as a dynamic, crystalline process rather than an episodic nuisance. One wonders, however, whether the emphasis on numerical targets may inadvertently depersonalize patient experience. After all, pain is not measured in mg/dL, though its absence often is.
Febuxostat costs what?! 😭
i had no idea tophi could actually shrink?! i thought they were permanent lumps. this gives me hope. my elbow looks like a marble collection now.
allopurinol is the OG gout killer and if your doc isn't pushing you to 400+ mg you're getting scammed