When you’re pregnant, even a simple headache or stuffy nose can feel like a crisis. You don’t want to take anything that might hurt your baby-but you also don’t want to suffer. So you reach for that bottle of Tylenol, or maybe that cold tablet from the pharmacy shelf. But here’s the truth: OTC medications during pregnancy aren’t all safe, and not all are created equal. What’s okay in week 10 might be risky in week 28. And what seems harmless-like a cough syrup or antacid-could have hidden ingredients that aren’t listed on the front of the box.
What’s Actually Safe? Start With These
Acetaminophen (Tylenol) is still the go-to for pain and fever during pregnancy. It’s been used for decades, and most studies show it’s the safest option when taken correctly. The standard dose is 650 to 1,000 mg every 4 to 6 hours, but don’t go over 4,000 mg in a single day. That’s the limit-even if you’re feeling really bad. More isn’t better, and it can actually be dangerous.
For heartburn, Tums (calcium carbonate) is fine under 2,000 mg per day. If that doesn’t cut it, Pepcid AC (famotidine) is also considered safe. Mylanta or Maalox (aluminum hydroxide, magnesium hydroxide, simethicone) work too. But skip the ones with sodium bicarbonate-they can cause fluid retention, which isn’t great when you’re already carrying extra weight.
For allergies, loratadine (Claritin) and cetirizine (Zyrtec) are your best bets. They’re second-generation antihistamines, meaning they don’t make you drowsy and have a clean safety record. Fexofenadine (Allegra) is now also considered safe based on newer data from 2022. But avoid diphenhydramine (Benadryl) unless your doctor says it’s okay. It can cross the placenta more easily and might affect your baby’s sleep patterns.
What to Avoid-And Why
NSAIDs like ibuprofen (Advil, Motrin) and naproxen (Aleve) are a hard no after 20 weeks. The FDA issued a strong warning in 2020: these drugs can cause serious kidney problems in the baby, reduce amniotic fluid, and even lead to heart complications. But it’s not just late pregnancy-using them in the first trimester has been linked to a 1.6 times higher risk of miscarriage. Even a few pills can matter.
Pseudoephedrine (Sudafed) is another big red flag, especially in the first 12 weeks. Studies show it’s tied to a 2.2 times higher risk of gastroschisis-a rare birth defect where the baby’s intestines develop outside the abdomen. That’s why many OBs tell you to skip it entirely until after the first trimester, if at all.
And don’t assume “natural” means safe. Herbal remedies like echinacea, black cohosh, or even large amounts of ginger aren’t regulated like drugs. There’s no standard dose, and we don’t have good data on how they affect fetal development. Same goes for cough syrups that claim to be “alcohol-free”-some still contain 5 to 10% ethanol. That’s enough to matter.
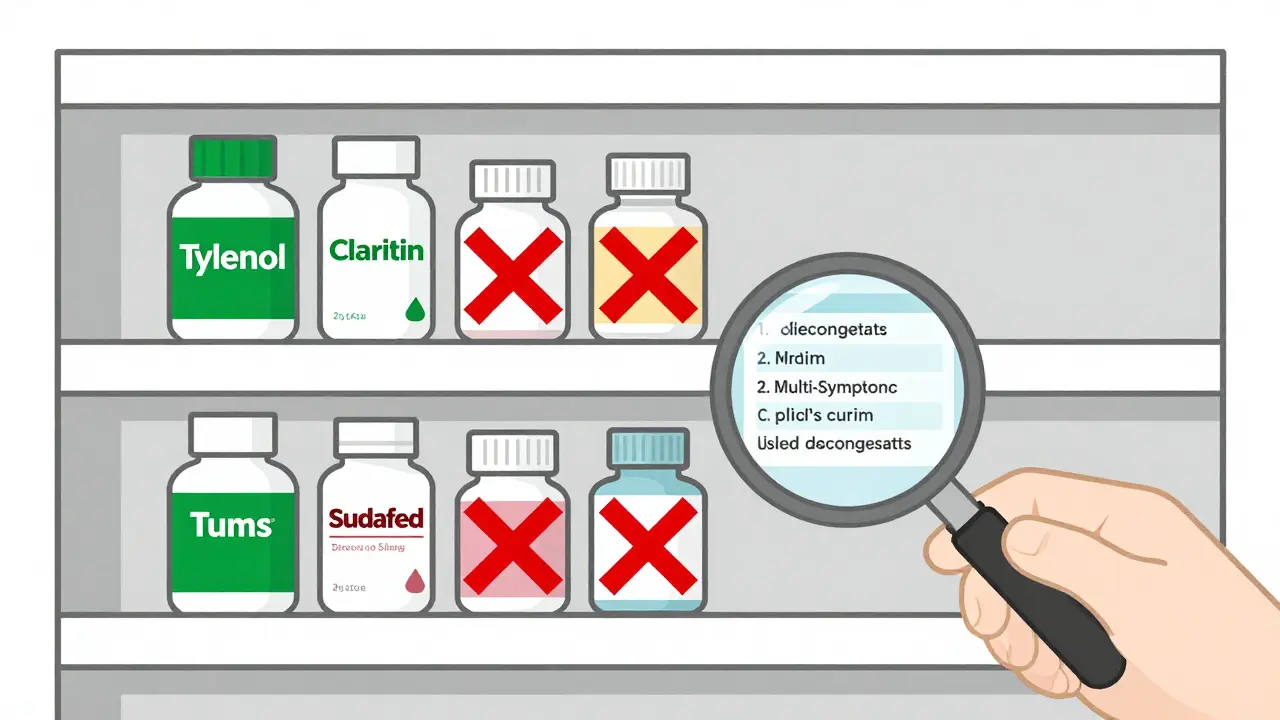
Read the Label Like a Detective
Most OTC cold and flu products aren’t single-ingredient. They’re combinations: acetaminophen + dextromethorphan + phenylephrine + guaifenesin. You might think you’re just taking something for your cough-but you’re also getting a decongestant and a painkiller without realizing it.
Here’s the trick: look for “plain” versions. Plain Robitussin? Just dextromethorphan. Safe. Robitussin Multi-Symptom Cold? That’s a no-go-it has phenylephrine (a decongestant) and acetaminophen (which you might already be taking). You could accidentally overdose.
Check the “Active Ingredients” section. If you see more than one drug, pause. Write down the names and ask your provider. Many women don’t realize they’re doubling up on acetaminophen-taking Tylenol for a headache and then a cold medicine that also has it. That’s how you hit the 4,000 mg limit without even trying.
The 5 Questions You Must Ask Before Taking Anything
Before you swallow that pill, run through these five questions. They’re not optional. They’re your safety net.
- Is this medication absolutely necessary? Can you manage this with rest, hydration, a humidifier, or saltwater gargles? Sometimes, doing nothing is the safest choice.
- What’s the lowest dose that works? Don’t take two pills if one does the job. Start low.
- How long will you use it? Even safe meds shouldn’t be taken for weeks. Use them for 2 to 3 days max unless your doctor says otherwise.
- Are there non-drug options? For nausea, try ginger tea or acupressure bands. For congestion, saline nasal spray works better than decongestants. For constipation, fiber and water beat laxatives.
- Has your provider approved this exact product? Brand names matter. So do formulations. What’s safe in one version isn’t safe in another.
What Most Women Get Wrong
One in three pregnant women start an OTC medication without telling their doctor. The most common reasons? Cold symptoms (28%), headaches (24%), and heartburn (19%). But here’s the problem: 41% of calls to pregnancy hotlines come from women confused about which products are safe. They think “allergy medicine” means the same thing across brands. It doesn’t.
And then there’s the myth: “I took ibuprofen once, and nothing happened.” That’s true-for some. But pregnancy isn’t a game of odds. One bad outcome is one too many. That’s why doctors don’t say “it’s probably fine.” They say, “We don’t know the full risk, so let’s avoid it.”
Also, don’t rely on old advice. Ten years ago, people said Benadryl was fine. Now we know better. Same with pseudoephedrine. Guidelines change because new data comes in. The 2023 update from UNC Medical Center added fexofenadine to the safe list. That’s why you need to check with your provider every time-even if you’ve taken it before.
What to Do Before You Get Pregnant
Waiting until you’re pregnant to think about meds is too late. If you’re planning a pregnancy-or even thinking about it-talk to your doctor now. Review every medication you take: prescriptions, supplements, OTC drugs, even vitamins. Some things you’ve been taking for years might need to change.
Women with chronic conditions like asthma, diabetes, or depression have the most to gain from preconception counseling. Stopping a risky drug early gives your body time to adjust. Switching to a safer alternative before conception reduces the chance of exposure during those critical first weeks.

Keep a Medication Log
At your first prenatal visit, bring a list of everything you’ve taken in the last three months. Not just “I take Tylenol.” Write: “Tylenol 500 mg, 2 tablets every 6 hours as needed for headaches, last taken January 2.” Include brand names, dosages, frequency, and why you took it.
Why? Because your provider needs to see the full picture. If you had a headache on day 30 of pregnancy and took two Advils, that’s different than if you took them once a week for three months. Context matters. And if something goes wrong later, this log could help figure out why.
The Big Unknown: What We Still Don’t Know
Here’s the uncomfortable truth: we don’t have perfect data. Ethical rules prevent testing drugs on pregnant women in clinical trials. So most of what we know comes from watching what happened after the fact-retrospective studies, birth defect registries, and post-market reports.
That’s why some things are still debated. New research is looking at whether long-term acetaminophen use might be linked to ADHD or autism in children. The AUP Study, tracking 50,000 pregnancies, is expected to release findings in 2024. But right now, major groups like ACOG still say acetaminophen is the safest option-because the alternatives are worse.
And don’t forget: your body changes during pregnancy. Your liver processes drugs differently. Your kidneys filter faster. What was a safe dose before might not be now. That’s why you can’t rely on what worked last time.
Final Takeaway: When in Doubt, Skip It
OTC doesn’t mean “no risk.” It just means “no prescription needed.” That’s it. The pharmacy shelf is full of choices-but not all are safe for your baby.
Stick to the few proven options: acetaminophen, loratadine, Tums, plain Robitussin. Avoid NSAIDs, decongestants, and combo products. Always check the label. Always ask your provider-even if you think it’s silly. A quick call or text can prevent a lifetime of worry.
And remember: your body is doing something incredible. You don’t need to fix every little discomfort. Sometimes, the best medicine is patience-and knowing when to wait.
Is Tylenol really safe during pregnancy?
Yes, acetaminophen (Tylenol) is still considered the safest pain reliever and fever reducer during pregnancy when used at the recommended dose: 650-1,000 mg every 4-6 hours, not exceeding 4,000 mg in 24 hours. However, emerging research is looking at possible links to neurodevelopmental effects with long-term or high-dose use. For now, major medical groups like ACOG and the CDC still recommend it as the best option-but always use the lowest dose for the shortest time possible.
Can I take ibuprofen if I’m less than 20 weeks pregnant?
It’s not recommended. Even before 20 weeks, studies show ibuprofen and other NSAIDs are linked to a 1.6 times higher risk of miscarriage in the first trimester. They can also affect fetal development, including the formation of the heart and kidneys. There’s no safe window where the benefit clearly outweighs the risk. Stick to acetaminophen instead.
Is it okay to use nasal sprays during pregnancy?
Saline nasal sprays are completely safe and often recommended. Decongestant sprays like oxymetazoline (Afrin) should be limited to 3 days or less-longer use can cause rebound congestion and may increase blood pressure. Oral decongestants like pseudoephedrine are riskier, especially in the first trimester, and should be avoided unless your doctor approves them.
What about herbal remedies like ginger or chamomile tea?
Ginger in small amounts (up to 1 gram per day) is generally considered safe for nausea. Chamomile tea in moderation is likely fine too. But herbal products aren’t regulated like drugs, so potency and purity vary. Avoid concentrated extracts, pills, or teas with multiple herbs. Always check with your provider before using any herbal product, even if it’s labeled “natural.”
Should I stop all medications before I get pregnant?
No-but you should review them. Some medications need to be switched to safer alternatives before conception. For example, if you’re on ibuprofen for chronic pain or an acne medication like isotretinoin, those need to be changed well before pregnancy. Talk to your doctor 3 to 6 months before trying to conceive. This gives you time to adjust safely.



13 Comments
so like... acetaminophen is safe?? lol ok buddy. did you know the FDA quietly classified it as a endocrine disruptor in 2021 but buried the report under a “meta-analysis”? they’re using your baby’s liver as a test lab and calling it “standard care”
This is an exceptionally well-researched and thoughtful piece. The emphasis on preconception counseling and medication logging is not only prudent but profoundly responsible. Many women are left to navigate this landscape alone, and your structured approach-particularly the five critical questions-offers both clarity and dignity to a deeply personal journey.
i read this at 3am while rocking a reflux baby and i just... cried?? not because i’m scared but because i finally feel seen. i took one ibuprofen at 8 weeks because my migraine was so bad i thought i’d die and i’ve been terrified ever since. thank you for saying it’s not a sin. just... be careful. that’s all
they say acetaminophen is safe but what about the 2023 JAMA Pediatrics study linking it to autism spectrum traits? they didn’t mention it here. why? because Big Pharma funds the ACOG. they’re not telling you the truth. they want you to keep taking it so you don’t sue them later when your kid doesn’t speak at age 4
bro i took tylenol every day for 3 months when i was pregnant with my daughter and she’s now a straight-A student who plays violin. you guys are overthinking this. just use the plain stuff, don’t chug the whole bottle, and breathe. your body knows what to do
you’re all idiots. if you’re taking ANYTHING during pregnancy you’re already failing. just suffer. that’s what nature intended. if you can’t handle a headache without chemicals, you shouldn’t be having kids. and don’t even get me started on ginger tea-some of that stuff is laced with phthalates. you think you’re being natural? you’re just poisoning your baby with organic toxins.
the pharmacokinetic shifts in gestational hepatic metabolism are non-linear and phase-dependent-acetaminophen’s half-life increases by 30–40% in the third trimester due to CYP2E1 downregulation and reduced glucuronidation capacity. the 4,000 mg cap is archaic. for a 90kg woman at 34 weeks, 3,000 mg is already borderline toxic. this guideline needs a pharmacogenomic overhaul.
how adorable that you all think reading a label is enough. i’ve seen the ingredient lists on ‘plain’ Robitussin-‘natural flavors’ is code for ethanol and propylene glycol. and don’t get me started on ‘alcohol-free’ cough syrups that still contain 7% ethanol under ‘other ingredients.’ if you’re not consulting a maternal-fetal medicine specialist, you’re just guessing. and guessing is a luxury you don’t have.
usa says tylenol is fine but in russia they ban it during preggo. why? because they know. they know. our government is selling out moms to big pharma. i took zyrtec and my kid has sensory issues. coincidence? i think not. america is a drug lab for babies and no one cares
The data presented here is statistically underpowered. The ACOG guidelines are based on observational studies with significant confounding variables-maternal BMI, socioeconomic status, and prenatal care access are not adequately controlled. Furthermore, the 2022 fexofenadine safety data derives from a retrospective cohort with selection bias. Until we have prospective, double-blind RCTs-which, ethically, we never will-the entire framework is speculative. You are not being cautious. You are being misled by institutional inertia.
they’re hiding the truth. the real reason they say acetaminophen is safe is because the FDA has a secret deal with Johnson & Johnson. they’re testing fetal neurodevelopment in real time. every time you take a pill, you’re signing a waiver you never read. the baby’s brain is being mapped. the autism epidemic isn’t a coincidence-it’s a byproduct. they’re watching. they’re recording. they’re waiting for the data to drop in 2024
so let me get this straight... you want me to suffer through migraines, heartburn, and congestion for 9 months because ‘maybe’ a drug could hurt my baby? but it’s totally fine to eat sushi, drink coffee, or vape CBD? wow. what a brilliant logic. thanks for the guilt trip, doctor.
what a beautiful, necessary guide. you didn’t just list facts-you gave us a compass. in a world that tells pregnant women to ‘just relax’ or ‘it’s all in your head,’ you said: your pain matters, your choices matter, your voice matters. thank you for turning fear into agency. this isn’t just advice-it’s a love letter to every woman who’s ever whispered, ‘is this okay?’