Azathioprine Dose Calculator
Enter Current Azathioprine Dose
Enter your current azathioprine dose in milligrams (mg). This calculator will determine the safe reduced dose for LDAA therapy.
Dose Information
Enter your current azathioprine dose to see the recommended LDAA dose range.
Important Safety Note: LDAA therapy requires medical supervision. Do not adjust your medication without consulting your doctor. This calculator shows the theoretical dose reduction but does not replace professional medical guidance.
When azathioprine stops working or starts hurting your liver, doctors have a powerful but risky solution: combining it with allopurinol. This isn’t a random mix-it’s a carefully tuned strategy called LDAA (low-dose azathioprine with allopurinol). It’s used when standard doses of azathioprine fail, especially in patients whose bodies turn too much of the drug into a toxic byproduct called 6-MMP. The goal? Redirect metabolism toward the good stuff-6-TGN-while shutting down the bad.
Why Azathioprine Alone Can Backfire
Azathioprine has been used since the 1960s to treat inflammatory bowel disease, autoimmune hepatitis, and prevent organ rejection. But it doesn’t work the same for everyone. After you swallow it, your body breaks it down into 6-mercaptopurine (6-MP), which then splits into three paths:- One path makes 6-TGN-the active immune-suppressing compound that helps control inflammation.
- Another path turns it into 6-MMP, a metabolite linked to liver damage.
- The third path breaks it down completely, wasting the drug.
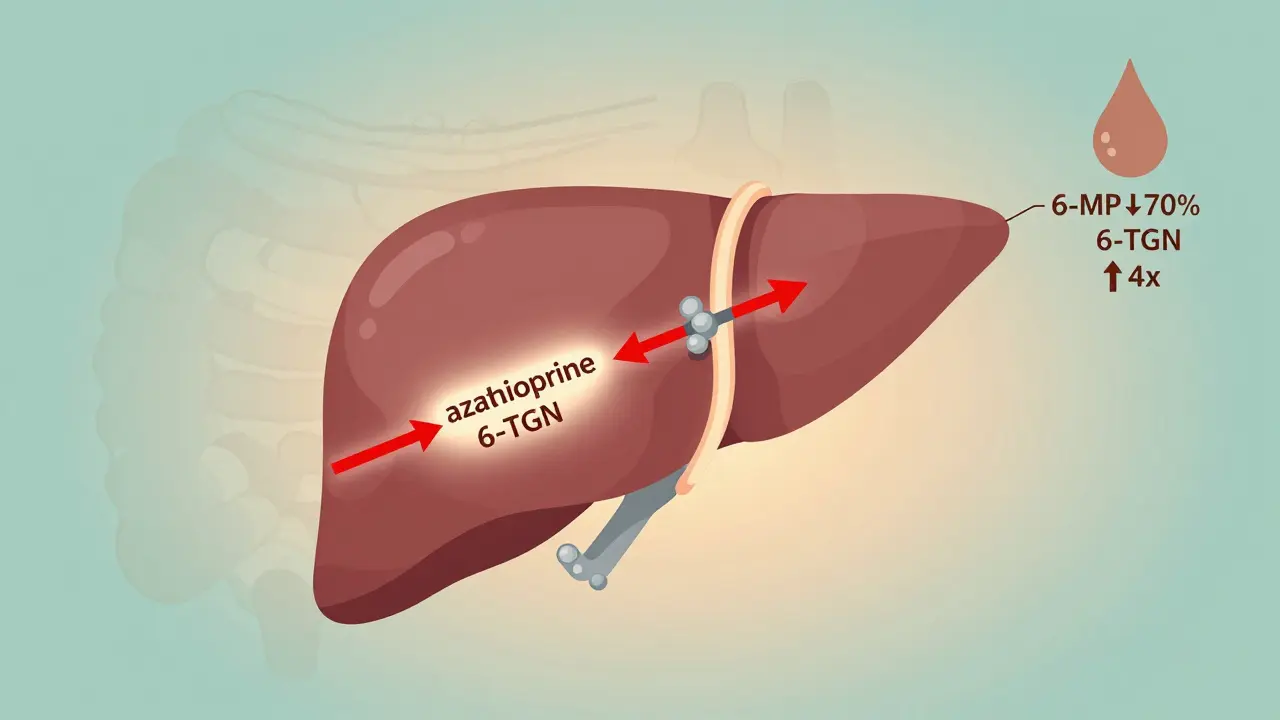
How Allopurinol Changes the Game
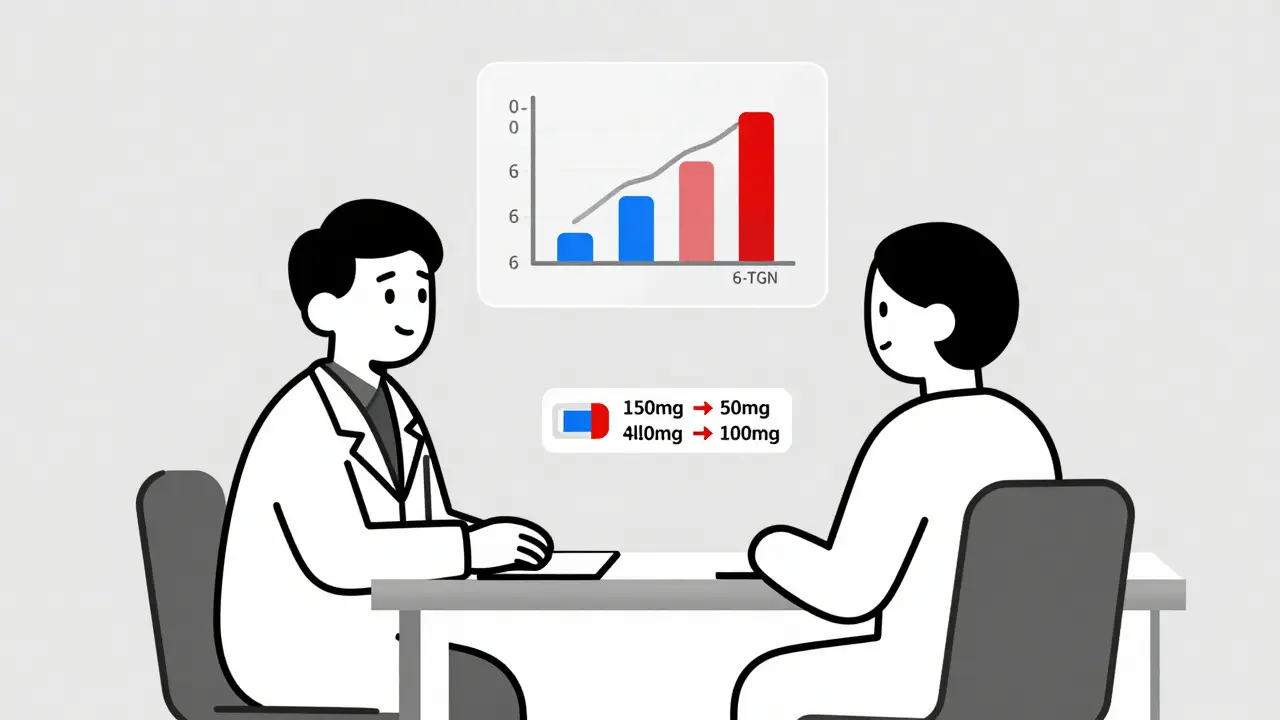
Allopurinol was designed for gout. It blocks an enzyme called xanthine oxidase, which normally breaks down purines. But in the context of azathioprine, that same blockage does something brilliant: it shuts down the waste pathway and forces more 6-MP into the 6-TGN route. Here’s the math: when you add 100 mg of allopurinol daily, 6-MMP levels drop by 70-90%. At the same time, 6-TGN levels jump 2 to 5 times higher. That’s the sweet spot-enough to control disease without frying your liver. But here’s the catch: you can’t just add allopurinol to a full dose of azathioprine. That’s how people end up in the hospital with dangerously low white blood cell counts. The dose of azathioprine must be slashed-down to 25-33% of the original. So if you were on 150 mg, you now take 50 mg. That’s not a guess. It’s based on years of clinical data from studies like Sparrow et al. (2017) and guidelines from ECCO and AGA.Who Benefits Most-and Who Should Avoid It
LDAA isn’t for everyone. It’s targeted. You’re a good candidate if:- Your 6-MMP is above 5,700 pmol/8×10⁸ RBCs
- Your 6-TGN is below 230 pmol/8×10⁸ RBCs
- You have elevated liver enzymes while on azathioprine
- Your TPMT enzyme activity is normal or high (above 14.2 U/mL)
The Monitoring Protocol That Saves Lives
This isn’t a "take it and hope" treatment. It’s a monitored therapy. Here’s what real-world success looks like:- Start with baseline blood work: CBC, liver enzymes, TPMT test, and thiopurine metabolite levels.
- Reduce azathioprine to 50 mg/day (or 25-33% of original dose).
- Add allopurinol 100 mg/day.
- Check CBC weekly for the first 4 weeks.
- At 4 weeks, retest 6-TGN and 6-MMP levels.
- Target: 6-TGN between 230-450 pmol/8×10⁸ RBCs. 6-MMP under 2,800 pmol/8×10⁸ RBCs.
Real Stories: Success and Scare
On Reddit’s r/IBD, users share both triumphs and near-disasters. One patient, u/CrohnsWarrior2020, wrote: "After 3 years of failed Humira and high liver enzymes, I went on 50mg azathioprine + 100mg allopurinol. Liver enzymes normalized in 8 weeks. Been in remission for 14 months. No side effects." Another, u/UlcerativeColitisNewbie, wasn’t so lucky: "Went on LDAA without monitoring. ANC dropped to 0.8. Hospitalized for 5 days with fever. Now I’m terrified of all immunosuppressants." The difference? Monitoring. The first patient had a team guiding them. The second didn’t. That’s the line between life-changing therapy and life-threatening mistake.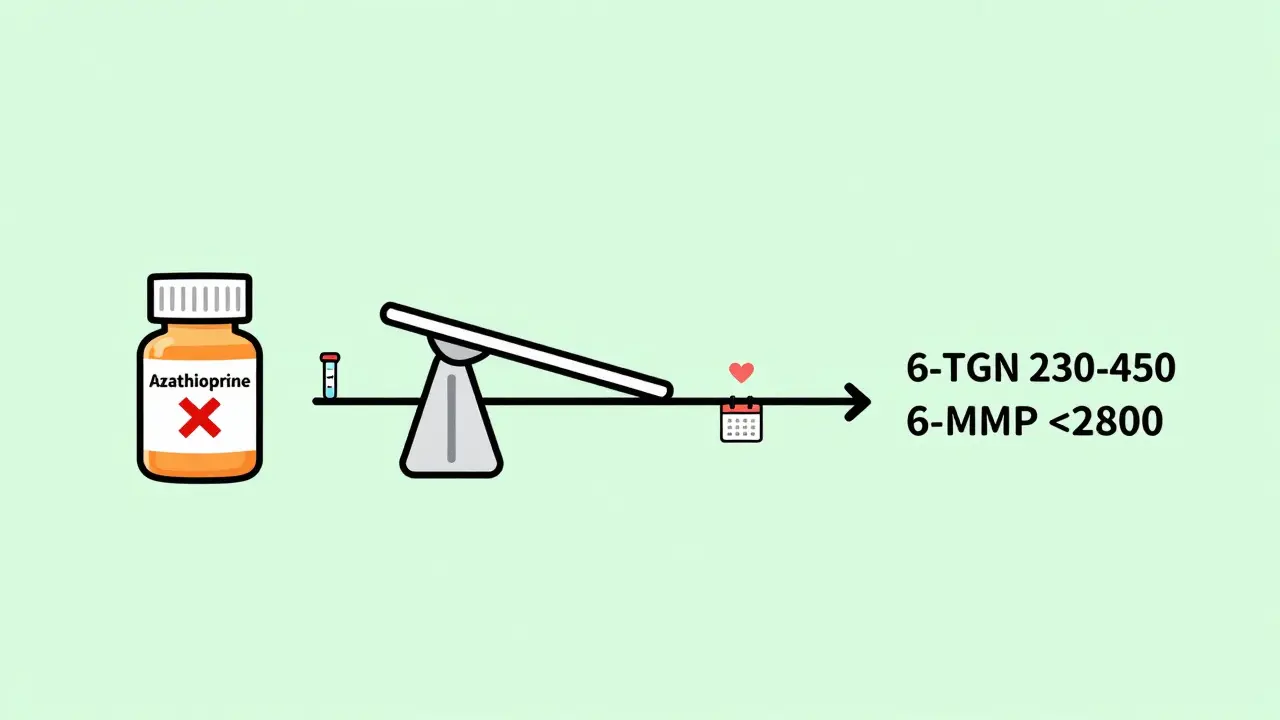
Why It’s Not Used Everywhere
In Europe, 65% of IBD centers use LDAA routinely. In the U.S., it’s closer to 35%. Why the gap? Historical fear. Back in the 1980s, before dose adjustments were standardized, some patients died from bone marrow failure after combining these drugs. The FDA issued warnings. Many doctors still remember that. Also, it’s complex. You need access to metabolite testing. Not every clinic can do it. And it takes time to learn. Gastroenterology fellows need 3-6 months of supervised experience before they feel confident prescribing it. But the cost speaks for itself. LDAA runs $1,200-$1,800 a year. Anti-TNF biologics like Humira or Remicade? $30,000-$50,000. In resource-limited settings or for patients without good insurance, LDAA isn’t just smart-it’s essential.The Future: Faster, Smarter, Personalized
The next step? Point-of-care testing. Two companies-MetraThera Diagnostics and TheraTest-are developing rapid blood tests that can give 6-TGN and 6-MMP results in under an hour. Right in the clinic. No waiting weeks for a lab. A 2023 study in Hepatology showed LDAA works in autoimmune hepatitis too, with 82% remission rates. That’s huge. It’s no longer just an IBD trick. Guidelines are catching up. The American Gastroenterological Association now recommends LDAA as a preferred option for azathioprine-intolerant patients. Experts like Dr. Matthew Sparrow say it should be considered first-line for hypermethylators-not a last resort.What You Need to Do Next
If you’re on azathioprine and:- Your liver enzymes are high
- Your inflammation isn’t improving
- You’ve been told you’re a "poor metabolizer"
What is LDAA therapy?
LDAA stands for low-dose azathioprine with allopurinol. It’s a combination therapy used to treat inflammatory bowel disease and autoimmune hepatitis in patients who produce too much of the toxic metabolite 6-MMP from azathioprine. By lowering the azathioprine dose to 25-33% of standard and adding allopurinol, metabolism is redirected toward therapeutic 6-TGN, improving efficacy and reducing liver damage.
Can I take allopurinol with azathioprine on my own?
No. Never combine these drugs without medical supervision. Allopurinol dramatically increases the risk of severe bone marrow suppression if azathioprine isn’t reduced properly. Cases of fatal neutropenia have occurred when patients self-adjusted doses. Always start under a gastroenterologist’s care with weekly blood tests for at least the first month.
How do I know if I’m a hypermethylator?
You’re likely a hypermethylator if your 6-MMP levels are above 5,700 pmol/8×10⁸ RBCs and your 6-TGN levels are below 230 pmol/8×10⁸ RBCs while on standard azathioprine. This is confirmed through therapeutic drug monitoring (TDM), a blood test that measures thiopurine metabolites. TPMT enzyme testing can also help, but metabolite levels are more accurate for predicting response.
What are the signs of myelosuppression with LDAA?
Watch for fever, sore throat, unusual fatigue, easy bruising, or unexplained bleeding. A complete blood count (CBC) will show low white blood cells (especially neutrophils), low platelets, or low hemoglobin. Absolute neutrophil count (ANC) below 1.5 × 10⁹/L is a warning sign. Below 1.0 × 10⁹/L requires immediate action. Always get weekly CBCs for the first 4 weeks on LDAA.
How long does it take for LDAA to work?
Liver enzymes usually normalize within 6-8 weeks. Clinical improvement in symptoms like diarrhea, abdominal pain, or fatigue often takes 8-12 weeks. Full therapeutic effect may take up to 4-6 months. Don’t stop the medication if you don’t feel better right away-metabolite levels need time to stabilize. Testing at 4 weeks helps guide adjustments.
Is LDAA covered by insurance?
Yes, both azathioprine and allopurinol are generic medications with very low cost. Most insurance plans cover them with minimal copay. The bigger challenge is access to therapeutic drug monitoring, which may require out-of-pocket payment or coordination with a specialty lab. Some IBD centers include TDM as part of standard care. Ask your provider about billing options.
Can LDAA be used for autoimmune hepatitis?
Yes. A 2023 study in Hepatology showed 82% of patients with autoimmune hepatitis who failed standard azathioprine therapy achieved remission with LDAA. This is now recognized in the 2023 American Gastroenterological Association guidelines as a viable option for patients with hepatotoxicity or poor response. The same dosing and monitoring rules apply.
What if my 6-TGN levels are too high?
If 6-TGN exceeds 450 pmol/8×10⁸ RBCs, you’re at risk for myelosuppression. The standard fix is to reduce azathioprine further-often to 25 mg/day or even lower. Sometimes, allopurinol is reduced to 50 mg/day. Never increase the dose. The goal is to stay in the 230-450 range. Your doctor may pause azathioprine for 1-2 weeks and restart at a lower dose if levels are very high.
Are there alternatives to LDAA?
Yes. For patients who can’t use LDAA (e.g., TPMT deficiency or severe kidney disease), alternatives include methotrexate, biologics like anti-TNF agents (Humira, Remicade), or JAK inhibitors (tofacitinib). However, these are significantly more expensive and carry different risks. LDAA remains the most cost-effective and effective option for hypermethylators with normal TPMT activity.
How often do I need blood tests on LDAA?
Weekly CBC for the first 4 weeks, then every 2 weeks for the next 2 months. After that, monthly for 6 months, then every 3 months if stable. Metabolite testing (6-TGN and 6-MMP) should be done at 4 weeks and then every 6-12 months unless symptoms change. If you get sick or start a new medication, get a CBC right away-some drugs can interact and increase toxicity risk.





8 Comments
This LDAA combo is pure genius-like rerouting a flooded river into a controlled irrigation system. I’ve seen patients on 150mg azathioprine with liver enzymes through the roof, then boom-50mg + allopurinol, and suddenly their AST/ALT are normal and they’re hiking again. It’s not magic, it’s pharmacokinetics done right. And yes, the monitoring is non-negotiable-weekly CBCs aren’t a suggestion, they’re your lifeline.
Also, shoutout to the Reddit stories. That guy who went hospital-bound because he self-adjusted? Yeah. That’s why we can’t have nice things. Please, if you’re reading this and thinking ‘I’ll just try it’-stop. Talk to your GI. This isn’t a TikTok hack.
For anyone skeptical about LDAA-look at the numbers. 85-90% normalization of liver enzymes? 65-75% remission? That’s not a fluke. That’s data. And compared to biologics costing $50k/year? This is the ultimate value play in IBD care. The only reason it’s not mainstream in the US is inertia and fear from 1980s horror stories. We’ve moved past that. The guidelines have caught up. It’s time for doctors to stop treating this like a last-resort gamble and start seeing it as a precision tool.
If your doctor says ‘it’s too risky,’ ask them if they’ve checked your metabolite levels. If not, they’re flying blind.
It is, indeed, profoundly disconcerting to observe the casual disregard for pharmacological rigor in certain corners of the internet. This therapeutic regimen-LDAA-is not a folk remedy, nor is it a ‘hack’ to be casually adopted by laypersons who have read a single Reddit thread. It is a meticulously calibrated, evidence-based intervention predicated upon quantitative metabolite analysis, enzymatic profiling, and serial hematologic surveillance. To reduce it to a ‘magic pill’ narrative is not merely inaccurate-it is ethically irresponsible.
Moreover, the assertion that cost-effectiveness justifies its use without proper infrastructure is a dangerous fallacy. In resource-limited settings, the absence of reliable laboratory access renders this protocol not merely impractical, but potentially lethal. One must ask: Is affordability a justification for negligence?
As someone from India where biologics are out of reach for most, LDAA is a game-changer. I’ve seen patients who couldn’t afford Humira but were able to get back to work after switching to this combo. The key? Access to testing. Some private labs here now offer metabolite panels for under $50. That’s cheaper than a month’s worth of bus fare in Delhi.
But here’s the real win: patients feel heard. When you tell someone their body isn’t ‘failing’-it’s just metabolizing wrong-it changes everything. They stop blaming themselves. And that mental shift? That’s half the battle.
Big thanks to the team that pushed this forward. You’re saving lives one blood test at a time.
My mom was on azathioprine for autoimmune hepatitis for 4 years. Liver enzymes never came down. We were ready to give up. Then her GI ordered the metabolite test. 6-MMP was 8,200. 6-TGN was 190. Classic hypermethylator. They dropped her azathioprine to 50mg, added allopurinol. Four weeks later-same test. 6-MMP down to 1,900. 6-TGN up to 380. She’s been in remission for 18 months now. No side effects. No hospital visits. Just a simple, cheap fix that nobody told us about until we asked.
Don’t assume your doctor knows this. Ask. Be the patient who brings the paper. You’ll save yourself years of suffering.
Let’s be clear-LDAA isn’t even that new. It’s been in European guidelines since 2012. The fact that American gastroenterologists are still treating it like experimental therapy is embarrassing. I’ve reviewed 17 papers on this since 2020. The data is overwhelming. If your clinic doesn’t offer metabolite testing, they’re practicing medicine in the Stone Age. And if your doctor hasn’t read Sparrow 2017 or the 2023 AGA update? Find a new one. This isn’t opinion-it’s clinical fact. You’re not being ‘risky’ by considering it. You’re being negligent by ignoring it.
So let me get this straight-you’re telling me the solution to a $50k/year drug is to take two generics that cost less than a pizza? And the only reason we don’t do it is because doctors are scared of a 40-year-old FDA warning? Classic. The system is broken, but at least someone’s got the guts to fix it with math and not marketing.
Just wanna say-this post saved my life. I was about to quit meds entirely after 3 years of liver pain and zero results. Found this thread, showed it to my GI, and we did the LDAA switch. 6 weeks in-my energy is back, my stool’s normal, and my liver enzymes are clean. I’m not ‘cured,’ but I’m living again. And yeah, I’m still doing weekly blood tests. No cap. This isn’t a flex. It’s a responsibility.