How CGMs Work: More Than Just a Blood Sugar Test
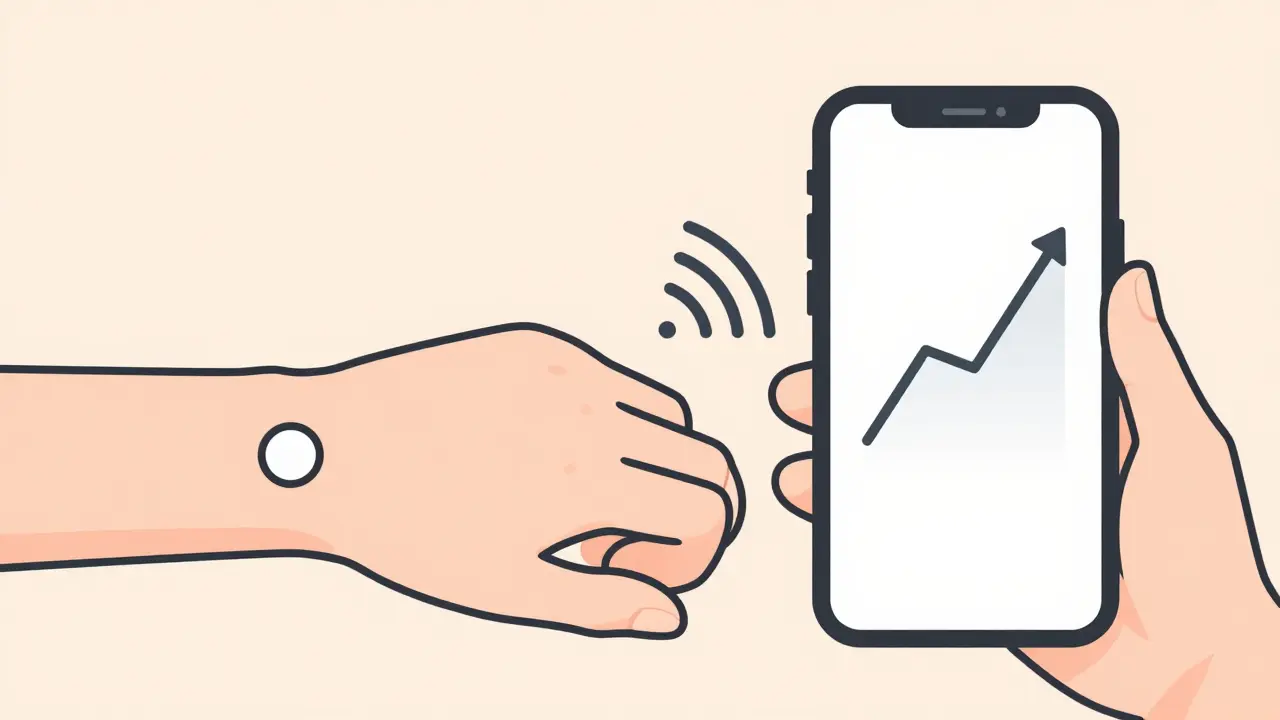
Continuous Glucose Monitors (CGMs) are medical devices that track blood sugar levels 24/7 without constant finger pricks. Unlike traditional glucose meters, CGMs measure sugar in the fluid between your cells (interstitial fluid) using a tiny sensor inserted under your skin. This sensor sends real-time data to your smartphone or receiver, giving you a constant stream of information about your glucose trends.
Imagine waking up in the middle of the night to a vibrating alarm on your arm. Your blood sugar is dropping dangerously low, but you're safe. This is the reality for millions using CGMs today. These devices don't just show your current number-they reveal patterns, warn of upcoming lows or highs, and help you make smarter decisions about food, exercise, and medication.
The Three Parts of a CGM System
Every CGM has three simple components working together:
- A tiny sensor (about the size of a coin) inserted under your skin, usually on your belly or arm. This sensor has a thin filament that measures glucose in the interstitial fluid.
- A transmitter that clips onto the sensor. It sends data wirelessly to your phone or receiver.
- Your phone or receiver that shows real-time numbers, trend arrows, and alerts. Apps like Dexcom Clarity or LibreView turn this data into easy-to-read graphs.
Dexcom G7 measures glucose every 5 minutes and lasts 10 days. FreeStyle Libre 3 updates every minute and stays on for 14 days. Eversense E3 is implanted under the skin and works for 6 months. All these devices use glucose oxidase enzyme in the sensor to react with sugar in your fluid, creating an electrical signal that gets converted into a reading.

Who Benefits Most from a CGM?
CGMs aren't just for people with type 1 diabetes. The American Diabetes Association recommends them for:
- Type 1 diabetes patients-especially those on insulin. A 2022 JAMA study of 32 clinical trials showed CGMs reduce severe low blood sugar episodes by 31% and lower A1C levels by 0.5-0.8% on average.
- Type 2 diabetes patients on insulin-who need precise dosing adjustments. Real-time data helps avoid dangerous lows during sleep or exercise.
- People with hypoglycemia unawareness-who don't feel symptoms of low blood sugar. Alarms can save lives.
Even non-diabetics use CGMs for wellness, but insurance rarely covers this. Most insurance plans only pay for CGMs if you have diabetes and take insulin. In the UK, the NHS covers FreeStyle Libre 2 for eligible patients at no cost. In the US, Medicare covers Dexcom and Medtronic devices for insulin users, but you'll still pay out-of-pocket without insurance.
Real-World Advantages Over Fingerstick Testing
Traditional blood glucose meters only show a single number at a time. CGMs give you a full story:
- Trend arrows show if your sugar is rising or falling fast. This is more important than the current number itself-Dr. Anne Peters, director of USC's Clinical Diabetes Programs, calls this "the most critical insight" for managing diabetes.
- Nighttime alerts prevent dangerous lows while you sleep. A Reddit user named u/Type1Since1995 shared: "My Libre 3 alarm saved me from a 32 mg/dL hypo at 3 AM last week-I'd have been dead without it."
- Patterns you'd never see. For example, a CGM might reveal your sugar spikes after eating certain foods, or drops after exercise. This helps tailor your diet and activity habits.

Limitations and Things to Watch For
CGMs aren't perfect. Here's what to expect:
- 5-20 minute lag. Glucose in interstitial fluid changes slower than in blood. During fast changes (like exercising), CGMs might not show the true blood sugar level yet. Always check with a fingerstick if you feel symptoms but the CGM says you're fine.
- Skin irritation. About 32% of negative reviews mention redness or itching at the sensor site. Using Skin Tac wipes or adhesive patches like Opsite Flexifix helps most people.
- False alarms. Dexcom G7 users report 22% of negative experiences involve unnecessary alerts during exercise. Some devices also react to acetaminophen (Tylenol), giving falsely high readings.
| Device | Measurement Frequency | Sensor Life | MARD | Cost (Monthly) | Key Features |
|---|---|---|---|---|---|
| Dexcom G7 | Every 5 minutes | 7 days | 9.1% | $399 | Real-time alerts, requires calibration |
| FreeStyle Libre 3 | Every 1 minute | 14 days | 7.9% | $110 | No fingerstick needed, automatic scanning |
| Eversense E3 | Every 1 minute | 180 days | 8.5% | Surgical implant required | Long-term monitoring, vibration alerts |
What's Next for CGM Technology?
The field is moving fast. In 2023, Dexcom launched the G7 with a 30-minute warmup (down from 2 hours). Abbott's FreeStyle Libre 3 Plus now tracks insulin doses. Future innovations include:
- Non-invasive sensors. Glucowise's optical sensor completed Phase 2 trials in September 2023, promising fingerstick-free monitoring.
- Multi-analyte patches. Sano Health's device measures ketones and lactate alongside glucose-ideal for people with type 1 diabetes at risk of ketoacidosis.
- Predictive closed-loop systems. Tandem's Control-IQ 3.0 (expected Q2 2024) will automatically adjust insulin 30 minutes before a low happens.
Apple's rumored glucose-monitoring smartwatch could disrupt the market too. But the biggest change isn't hardware-it's how CGMs integrate with other health tools. Your insulin pump, fitness tracker, and nutrition app might soon share data seamlessly, creating a full picture of your health.
How accurate are CGMs compared to fingerstick tests?
CGMs measure glucose in interstitial fluid, which lags behind blood glucose by 5-20 minutes. Modern devices like FreeStyle Libre 3 have a MARD (Mean Absolute Relative Difference) of 7.9%, and Dexcom G7 has 9.1%. This means they're reliable for trends but should be verified with a fingerstick during rapid changes (like exercise) or when symptoms don't match readings.
Can CGMs replace fingerstick tests completely?
Not yet. While FreeStyle Libre 3 and Dexcom G7 are FDA-approved as "non-adjunctive" (meaning they don't require fingerstick confirmation for most decisions), you still need a fingerstick during rapid glucose changes, when symptoms don't match readings, or if the CGM shows an error. Always double-check with a meter if you feel shaky, sweaty, or confused.
Are CGMs covered by insurance?
In the US, Medicare covers Dexcom and Medtronic CGMs for insulin-treated diabetics. Private insurance varies-most cover CGMs for type 1 diabetes but may require proof of insulin use for type 2. In the UK, NHS provides FreeStyle Libre 2 to 550,000 eligible patients at no cost. Without insurance, costs range from $110/month (Libre 3) to $399/month (Dexcom G7).
How long does a CGM sensor last?
Sensor life varies: Dexcom G7 lasts 7 days, FreeStyle Libre 3 lasts 14 days, and Eversense E3 lasts 180 days. Some devices like the Eversense require minor surgery for insertion and removal. Always follow manufacturer guidelines-overusing a sensor can cause inaccurate readings or skin irritation.
Do CGMs work during exercise?
Yes, but with caveats. During intense exercise, blood glucose changes faster than interstitial fluid, so CGMs may lag by 15-20 minutes. This is why you should check with a fingerstick if you feel symptoms of low blood sugar while working out. Some users report false alarms during exercise-Dexcom G7 has a 22% negative review rate for this issue.
Can non-diabetics use CGMs?
Yes, but insurance won't cover it. Companies like Zoe Health sell CGMs for wellness tracking, but they're expensive ($300-$400/month) and not medically necessary. Most doctors don't recommend CGMs for non-diabetics because the risks (like anxiety from false alarms) outweigh benefits. Research shows 18% annual growth in non-diabetic users, but this is mostly self-funded.