Breastfeeding Medication Safety Checker
When you’re breastfeeding, taking a pill for pain, depression, or an infection isn’t just about you. It’s about your baby too. Every time you swallow a medication, a small amount can end up in your breast milk. But here’s the truth most people don’t tell you: breastfeeding and medications are almost always safe together. Less than 2% of infants experience any real side effects from drug exposure through breast milk, according to the CDC. That’s not a guess-it’s data from real-world monitoring of millions of breastfeeding families.
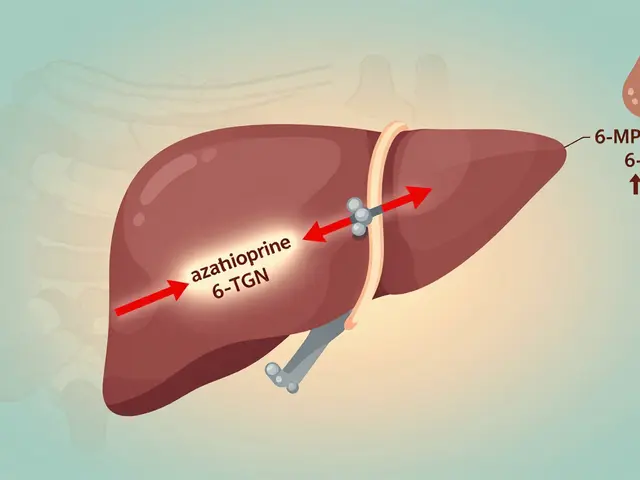
How Medications Actually Get Into Breast Milk
Medications don’t jump into your milk like water pouring into a cup. They move slowly, through passive diffusion, from your bloodstream into the milk-producing cells in your breasts. The process depends on four key things: molecular weight, lipid solubility, protein binding, and half-life.Small molecules under 200 daltons slip through easily. That’s why common painkillers like ibuprofen and acetaminophen pass through without trouble-they’re tiny. Big drugs, like insulin or heparin, barely make it into milk at all because they’re too large. Lipid solubility matters too. Fat-friendly drugs like some antidepressants or sedatives cross more easily. But if a drug is tightly bound to proteins in your blood (over 90%), it can’t get into milk. That’s why drugs like warfarin or phenytoin are low-risk.
Half-life is the big one. If a drug sticks around in your body for more than 24 hours, it builds up over time. That’s why some medications are safer to take once a day right after nursing-so your baby gets the lowest possible dose during their next feeding. And here’s something surprising: in the first few days after birth, your milk is colostrum, and you’re only making 30-60 milliliters a day. Even if a drug gets in, your baby barely gets any. By day five, your milk volume increases, but your body’s barriers tighten up, reducing transfer.
The L1 to L5 Risk System You Can Actually Trust
Dr. Thomas Hale created the most trusted system for judging medication safety during breastfeeding: L1 to L5. It’s not perfect, but it’s the best we’ve got.- L1 (Safest): Drugs like ibuprofen, acetaminophen, and most antibiotics (penicillin, cephalosporins). These have been studied in hundreds of mothers with no reported infant side effects.
- L2 (Probably Safe): Many antidepressants (sertraline, fluoxetine), antihypertensives (labetalol), and thyroid meds (levothyroxine). Some studies show tiny amounts in milk, but no harm.
- L3 (Possibly Safe): Drugs like benzodiazepines (lorazepam) or some ADHD meds (methylphenidate). Use with caution. Monitor baby for drowsiness or irritability.
- L4 (Possibly Hazardous): Lithium, cyclosporine, some chemotherapy drugs. Rarely used unless benefits clearly outweigh risks.
- L5 (Contraindicated): Only a handful-radioactive isotopes, some cancer drugs, ergotamine. These are exceptions, not the rule.
Here’s what you need to know: over 90% of commonly prescribed medications fall into L1 or L2. That’s not a marketing slogan-it’s what the data shows. You don’t need to stop breastfeeding because you need an antibiotic for a sinus infection. You don’t need to quit nursing because you’re on an SSRI for postpartum depression. In fact, stopping breastfeeding because of medication use is needed in less than 1% of cases, according to Dr. Ruth Lawrence’s research.
The Go-To Resources: LactMed vs. Hale’s Guide
You don’t need to guess. There are two trusted, free, evidence-based tools every breastfeeding parent and provider should know.LactMed, run by the U.S. National Library of Medicine, has data on over 4,000 drugs-including 350 herbs and 200 supplements added in 2021. It’s free, online, and updated monthly. It’s also technical. You’ll see plasma concentrations, milk-to-plasma ratios, and half-lives. It’s perfect if you’re a pharmacist or want to dig deep.
Hale’s Medications and Mothers’ Milk (2022 edition) is the clinical shortcut. It takes LactMed’s data and turns it into simple L1-L5 ratings. It’s what pediatricians and lactation consultants use at the bedside. It covers about 1,300 drugs, but it’s clearer. If you’re a mom looking for a quick answer, this is your best bet.
Both are better than Google. A 2021 study found that 78% of lactation consultants see at least one case per month where a mother was wrongly told to stop breastfeeding because of a medication. That’s not because doctors are careless-it’s because most weren’t trained in lactation pharmacology. LactMed gets over 1.2 million queries a year. That’s 3,300 searches a day. People are looking. They just need better access.
Timing and Dosing: Small Changes, Big Impact
You don’t need to avoid meds. You just need to time them right.If you’re taking a single daily dose, take it right after you nurse-especially if your baby sleeps longest at night. That gives your body time to clear the drug before the next feeding. For drugs taken multiple times a day, take them right before the feeding so the concentration peaks after your baby’s done eating.
Choose the shortest-acting version. For pain, use ibuprofen instead of naproxen. For sleep, pick lorazepam over diazepam. For antibiotics, amoxicillin beats doxycycline. Why? Because they clear faster. Also, avoid long-acting formulations. Extended-release pills stay in your system longer, meaning more drug leaks into milk over time.
Topical meds? Generally safer than pills. Creams, patches, and sprays rarely enter your bloodstream enough to reach milk-unless you put them directly on your nipple. In that case, wipe it off before nursing. That’s the only time you need to be extra careful.
What Medications Are Most Commonly Used?
You’re not alone. A 2022 study found that 56% of breastfeeding women take at least one medication. The top three categories:- Analgesics (28.7%)-ibuprofen, acetaminophen, codeine (in small doses)
- Antibiotics (22.3%)-amoxicillin, cephalexin, azithromycin
- Psychotropics (15.6%)-sertraline, fluoxetine, bupropion
Antidepressants are the most misunderstood. Many moms are told to stop breastfeeding because they’re on an SSRI. But sertraline has been studied in over 1,000 infants. Levels in milk are extremely low. Infants show no signs of sedation, poor feeding, or developmental delays. In fact, untreated maternal depression poses a far greater risk to the baby than the medication.
For opioids, codeine is risky because some moms metabolize it too quickly, turning it into dangerous levels of morphine. Oxycodone and hydrocodone are safer alternatives when needed. But even then, use the lowest dose for the shortest time.
What Should You Watch For in Your Baby?
Most babies show no reaction. But if you’re concerned, look for these signs:- Excessive sleepiness or difficulty waking to feed
- Poor feeding or decreased weight gain
- Unusual irritability or jitteriness
- Diarrhea or rash (rare)
If you notice any of these, don’t panic. Call your pediatrician or lactation consultant. Don’t stop breastfeeding unless they tell you to. Most of the time, it’s a temporary issue, or the medication can be switched.
Remember: if a drug is safe for your baby to take directly (like infant ibuprofen), it’s almost always safe through breast milk. The dose is just smaller.
The Future: Personalized Breastfeeding Pharmacology
Right now, we’re using broad guidelines. But the future is personal. The InfantRisk Center’s MilkLab study has measured actual drug levels in breast milk from over 1,250 mothers. They’ve found huge differences between women-even on the same drug.By 2030, we may be using genetic tests to predict how fast you metabolize a drug. Some people break down antidepressants slowly-so their milk has higher levels. Others clear them fast. With that data, we could tailor dosing to your body, not just averages.
The FDA is pushing drug companies to include breastfeeding women in clinical trials. Right now, only 12 of 85 FDA-approved biologics have any breastfeeding data. That’s changing. And apps like LactMed On-the-Go, with 45,000 downloads, are putting this info right in your pocket.
You don’t have to choose between being a healthy mom and being a breastfeeding mom. The science is clear: breastfeeding and medications can coexist. With the right info, you can keep doing what’s best for your baby-and for yourself.
Is it safe to take ibuprofen while breastfeeding?
Yes. Ibuprofen is classified as L1 (safest) for breastfeeding. It has a short half-life, low transfer into milk, and no documented side effects in infants. It’s one of the most recommended pain relievers for nursing mothers.
Can antidepressants affect my baby’s development?
No evidence shows that antidepressants like sertraline or fluoxetine harm infant development. Studies tracking babies exposed through breast milk for up to two years found no differences in cognitive, motor, or behavioral outcomes compared to unexposed babies. Untreated maternal depression is far more likely to impact your baby’s development than the medication.
Should I pump and dump after taking medication?
Almost never. Pumping and dumping doesn’t speed up drug clearance from your body-it just removes milk that already contains the drug. The drug leaves your system through your liver and kidneys, not your breasts. Only in rare cases (like radioactive iodine therapy) is pumping and dumping recommended-and even then, only for a few hours.
Are herbal supplements safe while breastfeeding?
Many are not well studied. LactMed now includes 350 herbal products, but most lack safety data. Some, like fenugreek, may increase milk supply but can cause allergic reactions or low blood sugar in babies. Others, like St. John’s Wort, may interact with antidepressants. Always check LactMed before using any supplement.
What if my doctor says I must stop breastfeeding?
Ask for a second opinion. Most doctors aren’t trained in lactation pharmacology. Check LactMed or Hale’s guide yourself. If the medication is L1 or L2, you likely don’t need to stop. If it’s L4 or L5, ask if there’s a safer alternative. In 99% of cases, there is. Don’t let misinformation cost you your breastfeeding relationship.




11 Comments
i took ibuprofen for weeks after my c-section and my babe was totally fine. no drowsiness, fed like a champ. why do people panic so much??
so let me get this straight-we’ve got a whole L1-L5 system for meds in breast milk, but my OB still looked at me like i was asking to poison my kid when i asked about sertraline? 🤡
as a nurse in a neonatal unit, i’ve seen too many moms quit breastfeeding because they were told ‘it’s not safe’-when the drug was L1. please, if you’re unsure, check LactMed. it’s free, it’s science, and it’s not your doctor’s guess.
you’re not being reckless-you’re being informed. and that’s powerful.
indian mom here-my aunt told me to stop breastfeedin if i take any pill. now i’m like… why u always so scared? my baby is fine, i’m fine. lactmed is real. trust data not aunties.
sertraline is literally the gold standard for breastfeeding moms with depression. studies show zero developmental impact. yet so many moms are scared into stopping because someone said ‘better safe than sorry.’
but here’s the truth: the real danger isn’t the drug-it’s the silence, the stigma, the guilt. your mental health matters. your baby needs a happy, present mom more than a perfectly drug-free milk supply.
you’re not failing. you’re fighting.
the data you cite is cherry-picked. while L1 and L2 drugs are generally safe, the long-term neurodevelopmental studies are sparse. we’re talking about infants with developing blood-brain barriers. reducing exposure is prudent, not paranoid.
also, ‘99% of cases have alternatives’ is a misleading statistic. what if the alternative is ineffective? what if the mother’s condition deteriorates? this isn’t a simple checklist.
you mention ‘less than 2% of infants experience side effects’-but you don’t define ‘side effects.’ Is a slightly fussier baby a side effect? A minor rash? A temporary change in stool consistency? These are often dismissed as ‘normal’ when they’re not.
also, your source is the CDC-but they don’t conduct primary research on lactation pharmacology. you’re citing secondary data without transparency.
my wife was on sertraline for 8 months postpartum. baby slept great, gained weight, hit every milestone. we used the ‘take after nursing’ trick and never once panicked.
if you’re scared, talk to a lactation consultant-not your gyno who last read about breastfeeding in med school 15 years ago. seriously. LactMed saved our sanity. 🙏
you say ‘pump and dump is almost never needed’-but what about when you take a high-dose opioid for surgery? my friend did that and her baby got sleepy. she dumped for 24 hrs. guess what? baby was fine after. so maybe ‘almost never’ is still too broad?
also, why are you promoting herbal supplements? fenugreek gave my kid diarrhea and made me gassy as hell. don’t act like ‘natural’ means safe.
just wanted to say THANK YOU for this post 🙌
my doc told me to stop nursing when I got antibiotics for a UTI. I checked LactMed on my phone during the appointment. He changed his mind. 😤
you’re right-most providers aren’t trained in this. but we can change that. share this. save someone’s breastfeeding journey. 💪🍼
let me tell you about the science behind drug transfer-it’s not just molecular weight and lipid solubility. The pH gradient between maternal blood and milk also plays a role, especially for weak acids and bases. For example, acidic drugs like ibuprofen tend to concentrate less in milk because breast milk is slightly alkaline, so ionization reduces passive diffusion. That’s why even though it’s small, it doesn’t transfer as much as you’d think.
Also, the volume of distribution matters. Drugs with high Vd (like some antidepressants) are sequestered in maternal fat and tissue, so less is available to enter milk. That’s why sertraline, despite being lipid-soluble, has such low milk concentrations-it’s not just about size, it’s about where the drug wants to hang out.
And let’s not forget the infant’s metabolism. Babies under 3 months have immature liver enzymes, so even tiny amounts can linger longer. That’s why timing matters even more for newborns. Take meds right after a feed, and let the baby sleep through the peak.
Also, colostrum has higher protein content, which binds more drugs, reducing transfer. That’s why the first few days are actually the safest, even though milk volume is low. It’s not just about quantity-it’s about composition.
And for the record, the L1-L5 system? It’s based on clinical observations, not just pharmacokinetics. LactMed includes case reports, adverse event logs, and even unpublished data from lactation networks. That’s why it’s so robust.
And yes, genetic polymorphisms in CYP enzymes can change everything. One mom on sertraline might have 10x higher milk concentration than another on the same dose. That’s why future personalized dosing is so exciting. Imagine a breastfeeding app that says, ‘Your CYP2D6 genotype means you metabolize this drug slowly-take it post-feed, not pre.’
And don’t get me started on the FDA’s new push for inclusion of lactating women in trials. We’ve been excluding them for decades. It’s not just ethical-it’s scientific. How can we claim to understand drug safety if we’ve never studied the population that uses it most?
Bottom line: you’re not just a mom taking a pill. You’re a data point in a revolution. And that’s beautiful.