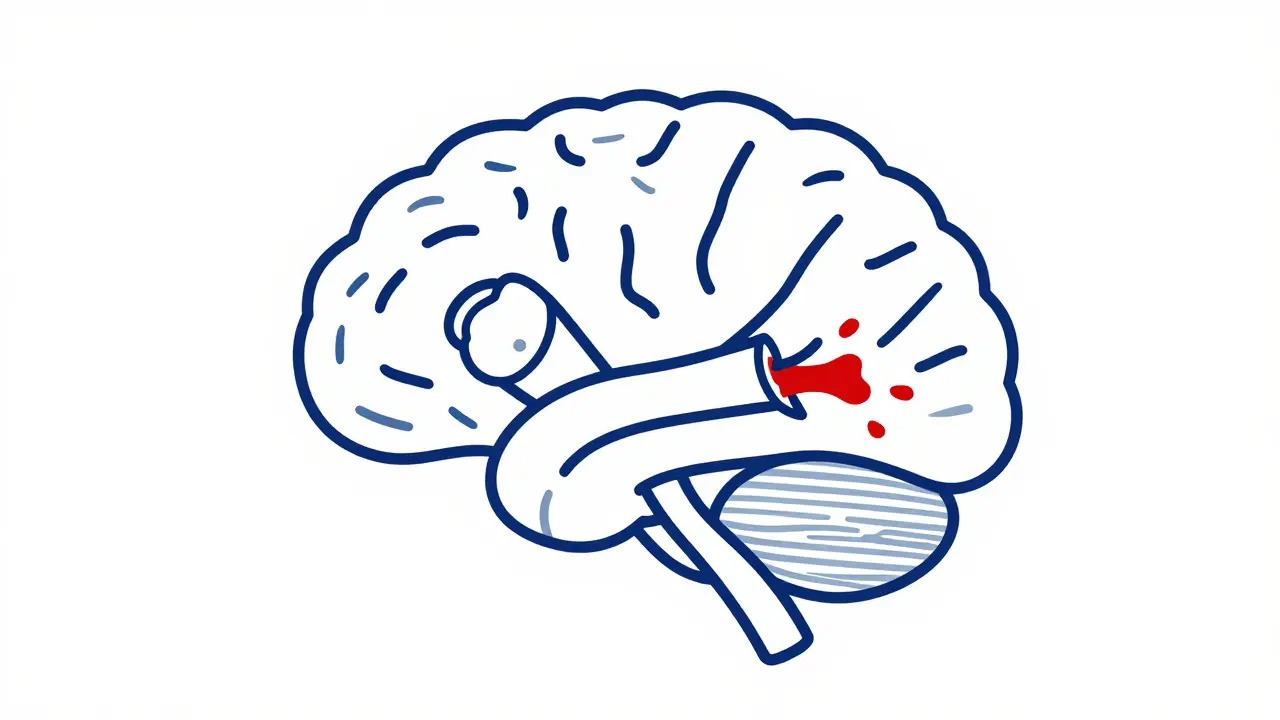
Every year, over 147,000 people in the US die from stroke. But here’s the thing: not all strokes are the same. There are two main types-Ischemic Stroke a blockage in a blood vessel supplying the brain, making up 87% of all stroke cases-and Hemorrhagic Stroke a ruptured blood vessel causing bleeding in or around the brain, accounting for 13-15% of strokes. Knowing the difference can mean the difference between life and death.
Understanding the Two Main Stroke Types
Ischemic strokes happen when a blood clot blocks blood flow to the brain. Think of it like a clogged pipe in a water system. The most common causes are fatty deposits in arteries (atherosclerosis) or clots traveling from the heart. Atrial fibrillation-a chaotic heart rhythm-increases embolic stroke risk by 500%, according to the American Heart Association. This type accounts for about 87% of all strokes.
Hemorrhagic strokes occur when a blood vessel bursts, flooding the brain with blood. This often results from uncontrolled high blood pressure or weakened blood vessels like aneurysms. While less common (13-15% of cases), hemorrhagic strokes are usually more severe. A 2022 Michigan Medicine review found they have higher immediate fatality rates than ischemic strokes.
How Symptoms Differ Between Stroke Types
Recognizing symptoms fast is critical. A 2017 Healthline study of 503 stroke patients revealed stark differences:
- Hemorrhagic strokes: 92.4% had severe headaches (vs. 19% in ischemic), 86.8% had dilated pupils (vs. 27.4%), and 17.4% had seizures (vs. 0%).
- Ischemic strokes: Gradual numbness or weakness on one side of the body, often worsening over minutes. Speech difficulties typically start as slurring before becoming complete loss.
On patient forums, ischemic stroke survivors often describe "sudden numbness spreading over 15-20 minutes" or "speech getting worse slowly." Hemorrhagic stroke survivors frequently report "explosive headaches like nothing before" and "immediate loss of consciousness."
Why Treatment Depends on the Stroke Type
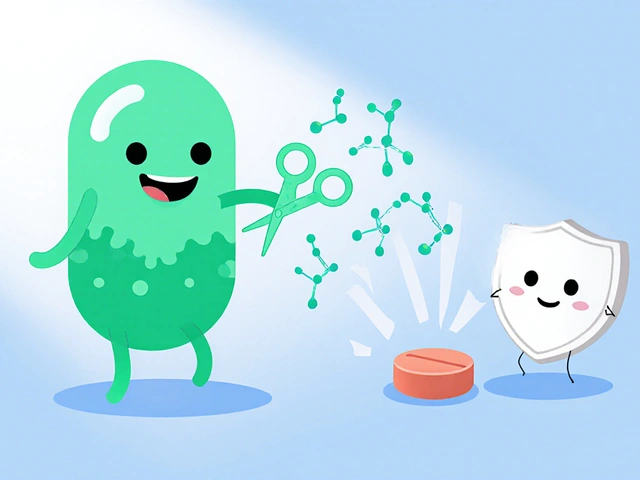
Time is brain-but treatment differs dramatically. For ischemic strokes, doctors use clot-busting drugs like tPA (alteplase) within 3-4.5 hours. A 2021 American Stroke Association guideline confirms this is the only way to dissolve the blockage. However, giving tPA to someone with a hemorrhagic stroke would be dangerous-it could worsen bleeding.
Hemorrhagic strokes often require surgery. Procedures like coiling (inserting tiny coils into an aneurysm) or clipping (placing a metal clip on the ruptured vessel) are common. A 2022 Stanford Medicine study found microsurgical clipping works better than coiling for certain aneurysm types. Controlling blood pressure is also critical to stop ongoing bleeding.
| Feature | Ischemic Stroke | Hemorrhagic Stroke |
|---|---|---|
| Prevalence | 87% of all strokes | 13-15% of all strokes |
| Primary Cause | Blocked blood vessel | Bleeding from ruptured vessel |
| Common Symptoms | Numbness, speech issues, gradual onset | Severe headache, vomiting, sudden loss of consciousness |
| Treatment | Thrombolytics (tPA), mechanical thrombectomy | Surgery to stop bleeding, blood pressure control |
Evidence-Based Prevention Strategies
Effective stroke prevention strategies depend on the type. For ischemic strokes, managing atrial fibrillation is key. Anticoagulants like apixaban reduce stroke risk by 60-70% in AFib patients, per the 2021 ARISTOTLE trial with 18,201 participants. Antiplatelet drugs like aspirin lower secondary ischemic stroke risk by 25%.
For hemorrhagic strokes, blood pressure control is the top priority. The SPRINT trial showed keeping systolic blood pressure below 120 mmHg (instead of 140) reduced hemorrhagic stroke risk by 38% in high-risk patients. Lifestyle changes matter too: the Mediterranean diet cuts overall stroke risk by 30% (PREDIMED study), and regular exercise (150 minutes weekly) lowers risk by 27%. Quitting smoking helps-stroke risk drops 50% within one year, according to CDC data.

Recognizing and Responding to Stroke Symptoms
The FAST Face drooping, Arm weakness, Speech difficulty, Time to call emergency services acronym is your best tool. A 2022 Stroke Patient Outcomes Report found 73% of positive outcomes happened when people called emergency services within 5 minutes of noticing symptoms.
Never drive yourself to the hospital during a stroke. Emergency responders can start treatment en route and alert the hospital. For ischemic strokes, they might administer tPA before arrival. For hemorrhagic strokes, they can monitor blood pressure and prepare for surgery. Every minute counts-delaying care increases brain damage.
Recent Advances in Stroke Care
Technology is changing stroke treatment. The 2023 WAKE-UP trial showed MRI-guided thrombolysis can extend treatment for ischemic strokes up to 9 hours, helping 20% more patients. For hemorrhagic strokes, minimally invasive surgery with alteplase reduced mortality by 10% in the 2022 MISTIE III trial.
Blood tests are also improving diagnosis. A 2023 study in the Journal of the American College of Cardiology found GFAP biomarkers distinguish hemorrhagic from ischemic strokes with 92% accuracy within 15 minutes. This could allow faster, more accurate treatment decisions even before reaching the hospital. Viz.ai’s AI platform, used in 1,200+ hospitals, reduces door-to-needle time for tPA by 52 minutes on average.
Can you have a stroke without symptoms?
Yes, "silent strokes" occur without noticeable symptoms but still damage brain tissue. These often go undetected until an MRI shows brain changes. While you might not feel sick, silent strokes increase future stroke risk and cognitive decline. Regular check-ups and managing risk factors like high blood pressure are crucial even if you feel fine.
What’s the FAST test and why does it matter?
FAST stands for Face drooping, Arm weakness, Speech difficulty, Time to call emergency services. It’s a quick way to spot stroke symptoms. If someone’s face droops on one side, can’t raise both arms, or has slurred speech, call 911 immediately. Acting fast gives doctors the best chance to treat the stroke before permanent damage occurs. Studies show patients who get help within 5 minutes of symptoms have significantly better outcomes.
Is it safe to drive yourself to the hospital during a stroke?
Never drive yourself during a stroke. Emergency medical services can start treatment en route and alert the hospital to prepare. For ischemic strokes, they might administer clot-busting drugs before arrival. For hemorrhagic strokes, they can monitor blood pressure and gather critical information. Driving yourself delays care and puts others at risk if symptoms worsen while driving.
How long do you have to get treatment for a stroke?
For ischemic strokes, clot-busting drugs like tPA are most effective within 3-4.5 hours of symptom onset. However, newer techniques like mechanical thrombectomy can work up to 24 hours for certain patients. Hemorrhagic strokes require immediate surgery to stop bleeding, so every minute counts. The "time is brain" principle applies to both types-delaying care increases brain damage and reduces recovery chances.
Can lifestyle changes really prevent strokes?
Absolutely. The PREDIMED study showed the Mediterranean diet (rich in olive oil, nuts, fruits, and vegetables) reduces stroke risk by 30%. Regular exercise lowers overall stroke risk by 27%, and quitting smoking cuts stroke risk in half within one year. For people with high blood pressure, controlling it through diet and medication can prevent up to 80% of hemorrhagic strokes. Prevention isn’t just possible-it’s within your control.