Cholesterol Reduction Calculator
Your Estimated LDL Reduction
0 mg/dL reduction
Your estimated LDL level: 0 mg/dL
Monthly cost (UK): -
Common side effects: -
When your doctor says you need a cholesterol‑lowering pill, it’s easy to assume all the drugs work the same way. In reality, each class has a distinct mechanism, effectiveness, and side‑effect profile. This guide walks you through Zetia (the brand name for ezetimibe) and the most common alternatives, so you can see which option fits your health goals and lifestyle.
Key Takeaways
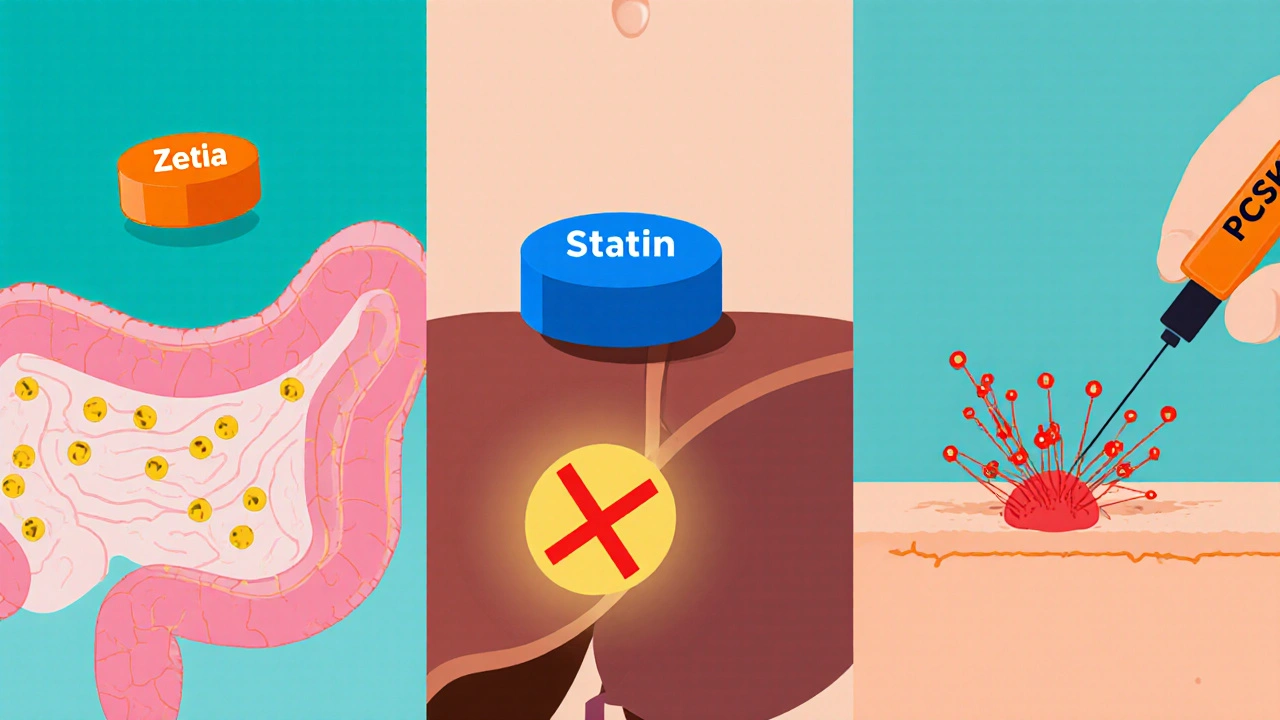
- Zetia blocks cholesterol absorption in the gut, yielding a modest 15‑20% drop in LDL‑C when used alone.
- Statins inhibit liver cholesterol production and typically lower LDL‑C by 30‑55%.
- PCSK9 inhibitors, though pricey, can cut LDL‑C by up to 60% and are injectable.
- Older agents like bile‑acid sequestrants and niacin are useful in specific scenarios but have adherence challenges.
- Choosing the right therapy depends on baseline LDL levels, cardiovascular risk, drug interactions, and cost.
Understanding How Each Drug Works
Zetia (Ezetimibe) is a selective inhibitor of intestinal cholesterol absorption. It binds to the Niemann‑Pick C1‑like 1 protein (NPC1L1) on the brush border of the small intestine, preventing dietary and biliary cholesterol from entering the bloodstream.
Statins are HMG‑CoA reductase inhibitors that curb the liver’s internal cholesterol synthesis. By reducing intracellular cholesterol, the liver pulls more LDL‑C from the blood, dramatically slashing levels.
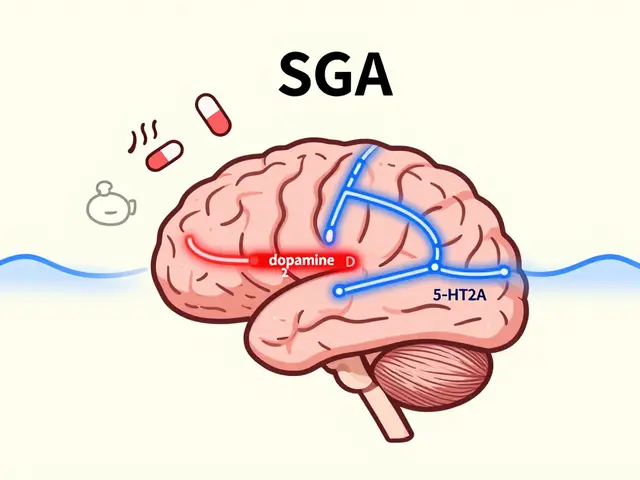
PCSK9 inhibitors (e.g., alirocumab, evolocumab) are monoclonal antibodies that block the PCSK9 protein, preserving LDL receptors on liver cells and boosting LDL clearance.
Bile‑acid sequestrants such as colesevelam bind bile acids in the intestine, forcing the liver to convert more cholesterol into bile acids, which lowers LDL‑C.
Niacin (nicotinic acid) works by inhibiting hepatic diacylglycerol acyltransferase‑2, reducing VLDL secretion and therefore LDL‑C, while also raising HDL‑C.
Efficacy at a Glance
| Drug/Class | Typical Dose | Mechanism | Average LDL‑C Reduction | Common Side Effects | Cost (UK, per month) |
|---|---|---|---|---|---|
| Zetia (Ezetimibe) | 10 mg daily | Inhibits intestinal cholesterol absorption | 15‑20 % | Diarrhea, mild liver enzyme rise | £15‑£25 |
| Atorvastatin (Statin) | 10‑80 mg daily | Blocks HMG‑CoA reductase | 30‑55 % | Muscle aches, raised CK, liver enzymes | £5‑£10 |
| Rosuvastatin (Statin) | 5‑40 mg daily | Blocks HMG‑CoA reductase | 40‑55 % | Myalgia, occasional gout flare | £7‑£12 |
| Alirocumab (PCSK9 inhibitor) | 75 mg sub‑Q bi‑weekly | Neutralises PCSK9 protein | 50‑60 % | Injection site reaction, flu‑like symptoms | ~£300 (NHS subsidy varies) |
| Colesevelam (Bile‑acid sequestrant) | 3.75 g daily | Binds bile acids in gut | 10‑15 % | Constipation, abdominal bloating | £12‑£18 |
| Niacin (nicotinic acid) | 500‑2000 mg daily | Inhibits VLDL secretion | 5‑15 % | Flushing, hyperglycaemia, liver toxicity | £8‑£14 |
Safety and Tolerability
Zetia’s side‑effect profile is generally mild. The most reported complaints are gastrointestinal - mainly loose stools that settle after a few weeks. Liver enzymes can creep up, so clinicians usually check ALT/AST after three months of therapy.
Statins are effective but carry a higher risk of muscle‑related issues. About 5‑10 % of users notice soreness; a small fraction develop rhabdomyolysis, especially when combined with certain antibiotics or fibrates. Regular monitoring of CK levels helps catch problems early.
PCSK9 inhibitors are injected subcutaneously and are well tolerated in trials. The biggest barrier is cost, not safety. A few patients report persistent injection‑site redness, but it rarely leads to discontinuation.
Bile‑acid sequestrants can be hard on the gut. Constipation is common, and they may interfere with the absorption of other oral meds, so timing matters. Niacin’s flushing can be uncomfortable; taking aspirin beforehand often blunts the reaction, but it still isn’t ideal for many patients.
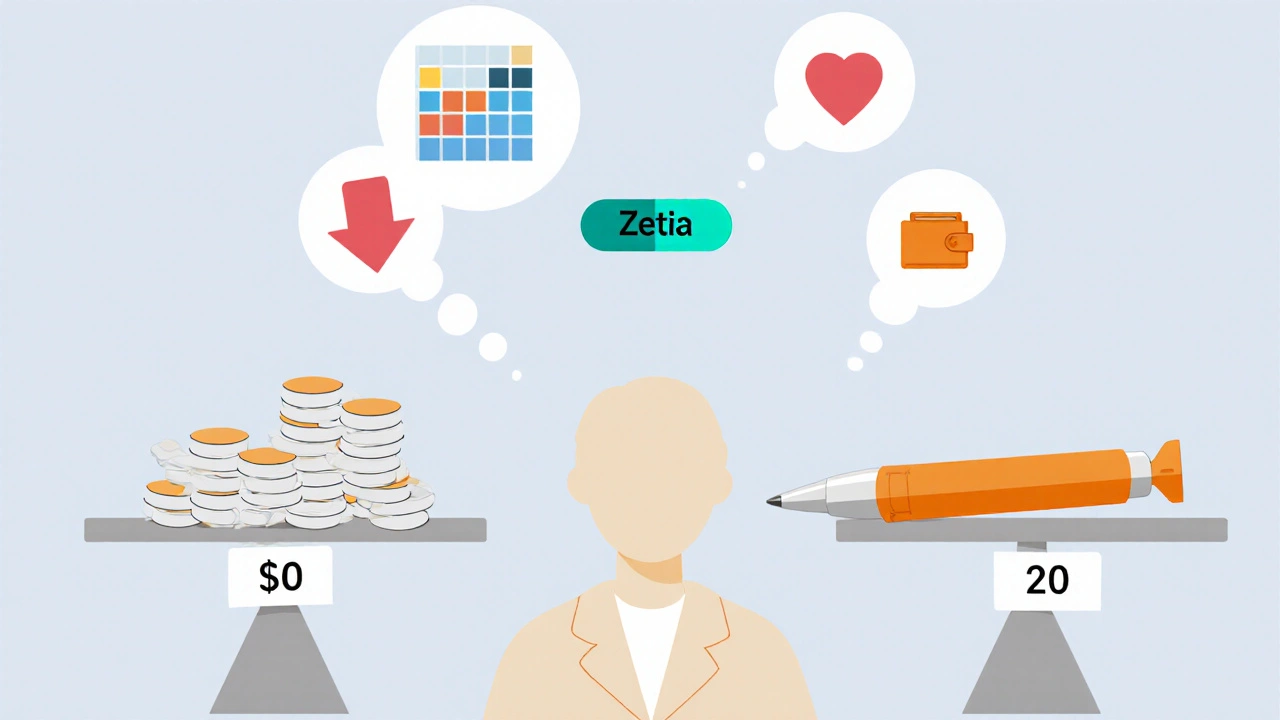
Cost Considerations in the UK
Prescription charges in England are £9.35 per item, but many patients qualify for free prescriptions under the NHS exemption criteria. Zetia, being a relatively new branded drug, often sits on the higher end of the pharmacy price list. Statins are mostly available as generics, making them the most budget‑friendly choice.
PCSK9 inhibitors are expensive, but the NHS funds them for high‑risk patients with familial hypercholesterolaemia or established cardiovascular disease who can’t reach targets with oral meds. If you fall outside those categories, you’ll likely face a co‑payment or need private insurance.
Bile‑acid sequestrants and niacin are cheap, yet their modest efficacy means they’re usually added only when the primary therapy isn’t enough.
How to Pick the Right Therapy
Start by looking at your baseline LDL‑C and overall cardiovascular risk. If you’re a primary‑prevention patient with moderately elevated LDL (130‑159 mg/dL) and no major risk factors, a moderate‑intensity statin might be enough. Add Zetia if you can’t tolerate higher statin doses or need a small extra push.
For secondary‑prevention patients - those who’ve already had a heart attack or stroke - guidelines push for intensive LDL reduction (<70 mg/dL). In that case, a high‑intensity statin plus either Zetia or a PCSK9 inhibitor is common.
If you have statin‑associated muscle pain that limits dosing, consider switching to a different statin, adding Zetia, or trying a bile‑acid sequestrant. For patients with very high baseline LDL (≥190 mg/dL) due to genetics, PCSK9 inhibitors or a combination of statin + Zetia may be the most effective route.
Don’t forget drug‑drug interactions. Zetia has few, but statins interact with certain anti‑infectives (e.g., clarithromycin) and fibrates. Niacin can raise blood sugar, so diabetics should use it cautiously.
Frequently Asked Questions
Can I take Zetia without a statin?
Yes, Zetia can be prescribed as monotherapy, especially for patients who can’t tolerate any statin. Expect a modest LDL‑C drop (15‑20 %) compared with the larger reductions seen with statins.
What is the biggest advantage of PCSK9 inhibitors over Zetia?
The main advantage is potency. PCSK9 inhibitors can halve LDL‑C levels, which is useful for very high‑risk patients. They’re injectable and pricey, while Zetia is a cheap pill with a gentler effect.
Do I need regular liver tests on Zetia?
A baseline liver panel is recommended, then a repeat after three months. If enzymes stay within normal limits, further testing isn’t usually required.
How does a bile‑acid sequestrant differ from Zetia?
Bile‑acid sequestrants act in the gut by binding bile acids, forcing the liver to use more cholesterol to make new bile. Zetia blocks cholesterol from entering at all. The sequestrants tend to cause constipation, while Zetia’s side effects are milder.
Is it safe to combine Zetia with a high‑intensity statin?
Combining the two is common practice and approved in the UK. The combo can achieve up to a 45‑50 % LDL‑C reduction, still with a low risk of serious side effects. Your doctor will monitor liver enzymes and muscle markers.
Bottom Line
Choosing a cholesterol‑lowering regimen isn’t a one‑size‑fits‑all decision. Zetia offers a gentle, well‑tolerated option that works well alongside statins or as a fallback when statins aren’t suitable. Statins remain the backbone of therapy for most patients because of their strong efficacy and low cost. PCSK9 inhibitors are the go‑to for high‑risk individuals who need the deepest LDL cut, while older agents like bile‑acid sequestrants and niacin have niche roles.
Talk to your GP or pharmacist about your personal risk profile, medication history, and budget. With the right information, you can land on a regimen that keeps your cholesterol in check without compromising quality of life.


9 Comments
When you’re staring at the LDL‑C numbers on a lab report it can feel like you’re watching paint dry, but there are real choices beyond just popping pills; diet, exercise, and genetics all play a part, and understanding how each drug fits into that puzzle can empower you to make better decisions.
First, remember that statins remain the workhorse for a reason: they target the liver’s cholesterol factory and can slash LDL by up to half, which is why guidelines put them front‑and‑center for high‑risk patients.
Ezetimibe, marketed as Zetia, works in the gut, stopping the absorption of about 15‑20 % of dietary cholesterol, and it’s especially handy when you can’t tolerate a high‑intensity statin dose.
Combination therapy – a low‑dose statin plus ezetimibe – often lands you right in the sweet spot of efficacy without the muscle pain that higher statin doses sometimes cause.
If cost is a concern, generic statins are usually pennies per month, while Zetia can be pricier, though many insurers will cover it if you have a documented statin intolerance.
PCSK9 inhibitors are a different animal: injectable, very effective, but they’re usually reserved for familial hypercholesterolemia or patients who have already maxed out oral options.
Don’t forget about the under‑appreciated role of lifestyle – soluble fiber, plant sterols, and omega‑3 fatty acids can modestly lower LDL and improve overall heart health.
For patients with borderline LDL levels, starting with a moderate‑intensity statin and adding a small dose of ezetimibe later can keep you under the target without breaking the bank.
Monitoring is key: liver enzymes for statins, ALT/AST for ezetimibe, and CK for any muscle symptoms, so schedule those labs at three‑month intervals after initiation.
Side‑effect profiles differ – statins may cause myalgia, while ezetimibe’s most common complaint is mild diarrhea that usually resolves on its own.
If you’re pregnant or breastfeeding, ezetimibe is generally avoided, whereas certain statins are also contraindicated, so talk to your OB‑GYN about the safest route.
Patients with diabetes need to watch for modest changes in glucose control with niacin, which is another reason ezetimibe is often preferred as an add‑on therapy.
In real‑world practice, adherence matters more than the theoretical LDL drop; a once‑daily pill that you actually take is better than a powerful drug you forget.
Finally, engage your primary care provider in shared decision‑making – bring up your concerns about side effects, cost, and lifestyle, and together you can craft a plan that feels sustainable for the long haul.
It is essential to recognize that the pharmacodynamics of ezetimibe differ fundamentally from HMG‑CoA reductase inhibition, thereby warranting a distinct therapeutic rationale; moreover, when statin tolerance is compromised, the additive LDL reduction achieved through combined therapy is both statistically and clinically significant, particularly in secondary‑prevention cohorts.
The guide glosses over the fact that many patients simply cannot afford PCSK9 inhibitors, making them a luxury rather than a viable option for the average person.
Ezetimibe works in the intestine preventing cholesterol absorption it is a modest option but useful when statins cause muscle pain the drug is generally well tolerated it does not require blood monitoring beyond initial liver enzymes the cost is higher than generic statins yet lower than injectable biologics patients often combine it with a low dose statin to achieve target LDL levels the combination is synergistic improving outcomes without increasing side effects the simplicity of a daily pill is a clear advantage over bi‑weekly injections adherence improves when dosing is straightforward many clinicians overlook ezetimibe as a first‑line add‑on despite solid evidence supporting its efficacy
Interesting read.
Ah yes, another glossy pharmaceutical pamphlet trying to make you feel empowered while quietly nudging you toward endless prescriptions, because nothing says "I care about your health" like a stack of brand‑name pills that will empty your wallet faster than a leaky faucet; the real miracle would be if doctors actually spent half the time they waste on marketing hype listening to patients instead of reciting drug monographs, but hey, who needs genuine conversation when you have brilliantly designed side‑effect tables to distract from the fact that lifestyle changes are still the most under‑utilized tool in our arsenal?
Honestly, if you’re not willing to invest in a "real" solution, you might as well stay stuck 😒💊💸.
Got you – it can feel overwhelming, but start small: add a fiber‑rich food a day and keep moving, and you’ll see progress without any fancy meds.
Remember, health is a journey, not a race; every positive step, no matter how tiny, builds a brighter future for your heart.