Since 2018, a quiet but dangerous problem has been creeping into generic medications millions of people rely on every day. It’s not a manufacturing error you can see. It’s not a labeling mistake. It’s something invisible - nitrosamine contamination - a group of chemical impurities that can cause cancer, even in tiny amounts. What started with a single recall of blood pressure meds has exploded into a global crisis affecting dozens of drugs, from antidepressants to diabetes pills. And the response from regulators hasn’t been simple. It’s been messy, evolving, and deeply stressful for manufacturers - especially small ones trying to keep prices low while keeping patients safe.
How Did Nitrosamines Show Up in Medications?
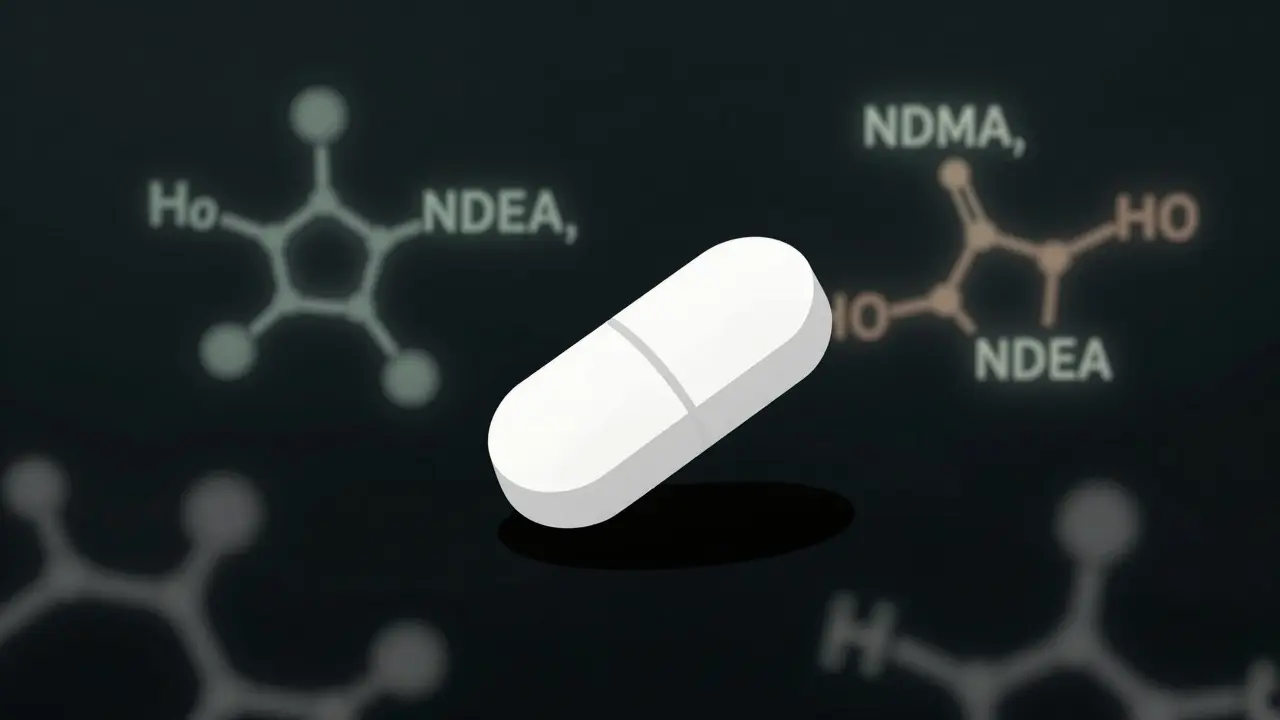
Nitrosamines aren’t added on purpose. They form by accident during manufacturing. When certain chemicals - like secondary amines - react with nitrites (often found in solvents, reagents, or even excipients like magnesium stearate), they create N-nitroso compounds. These are the nitrosamines. The problem isn’t new. Scientists have known about them for decades. But until 2018, no one was looking for them in pills. That changed when the FDA found NDMA - N-nitrosodimethylamine - in valsartan, a common blood pressure medication. NDMA is a known animal carcinogen and classified as a probable human carcinogen by the International Agency for Research on Cancer. The levels were low - measured in nanograms per pill - but enough to trigger immediate action. Within weeks, over 10 products were pulled from U.S. shelves. By mid-2025, more than 500 recalls had been issued across the globe, mostly in the U.S. It didn’t stop there. The same impurities showed up in losartan, ranitidine (Zantac), metformin, duloxetine, and even varenicline (Chantix). Each time, the source was different: a change in solvent, a new supplier of raw material, a shift in temperature during synthesis. Even packaging became a culprit. Blister packs and bottle liners containing secondary amines were found to release nitrosating agents over time, contaminating drugs during storage.What Are the Acceptable Limits? And Why Do They Matter?
The FDA doesn’t say “zero nitrosamines are safe.” Instead, they set acceptable intake (AI) limits based on lifetime cancer risk. For most common nitrosamines like NDMA and NDEA, the limit is 96 nanograms per day and 26.5 nanograms per day, respectively. But newer, more complex impurities - called NDSRIs (nitrosamine drug substance-related impurities) - have their own rules. For example, N-nitroso-varenicline has a limit of 96 ng/day, even though it’s structurally different from NDMA. Here’s where it gets tricky: if a pill contains more than one nitrosamine, you can’t just add up the individual limits. The FDA says the total risk must stay below the acceptable threshold. So if one impurity is at 80% of its limit and another is at 70%, you’re already over. That’s why testing isn’t just about checking for one compound - it’s about screening for dozens, simultaneously, at parts-per-billion levels. That requires advanced equipment: liquid chromatography-tandem mass spectrometry (LC-MS/MS). Not every lab can do it. And it’s expensive. A single batch test can cost hundreds of dollars. For a small generic maker running 20 products, that’s $500,000 to $2 million a year just in testing.The FDA’s Changing Rules - And Why They Matter
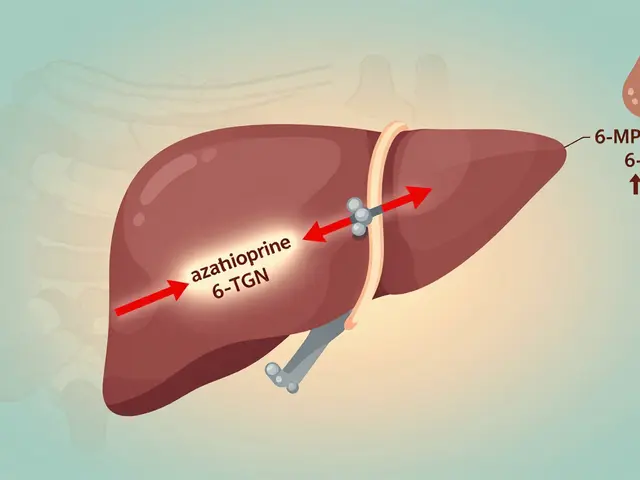
In August 2023, the FDA dropped a bombshell: all manufacturers had to prove they had control strategies in place by August 1, 2025. That meant reformulating products, changing suppliers, validating new processes - all while keeping supply flowing. But by June 2025, they backed off. Instead of requiring full compliance by the deadline, the FDA now asks companies to submit progress reports in their annual filings. They’re not giving up - they’re acknowledging reality. One manufacturer spent 18 months and $2 million just to fix nitrosamine formation in their metformin line. Another had to replace an entire batch of magnesium stearate because one supplier’s material contained hidden nitrites that triggered NDEA formation across three different drugs. The shift reflects a deeper truth: nitrosamine contamination isn’t a single problem. It’s a web. Fix one pathway, and another opens. A change in drying temperature might eliminate NDMA but create NTTP. Switching solvents might remove one impurity but introduce another. That’s why the FDA’s latest guidance stresses root cause analysis - not just testing.
Who’s Getting Hit the Hardest?
Large manufacturers like Teva, Sun Pharma, and Fresenius Kabi have the resources to absorb the cost. They have in-house analytical labs, global supply chains, and legal teams to navigate FDA requests. But smaller companies? They’re being squeezed. One European API supplier told a PharmaTech forum they lost three major clients because they couldn’t afford to revalidate their processes. Another U.S. generic maker shut down a profitable line because the cost to fix nitrosamines exceeded the profit margin on the drug. The result? Fewer generic options. Shortages. Higher prices. From 2018 to 2020, 15-20% of ARB products were temporarily unavailable in the U.S. due to recalls. That’s not just inconvenience - it’s a health risk for patients who rely on those meds daily. And while big players can absorb the hit, smaller ones are disappearing. Evaluate Pharma estimates the industry’s profit margins dropped 3-5 percentage points between 2020 and 2025 because of compliance costs.What’s Working? Real Stories From the Front Lines
Not all stories are grim. Some manufacturers got ahead of the curve. One company developing a new generic antidepressant ran nitrosamine risk assessments during early development. They found a potential pathway involving a common excipient and switched to a different one - before ever launching the product. No recall. No public scare. No lost sales. Another firm invested in training their chemists and analysts early. They built a database of nitrosamine formation risks for common drug structures. Now, they can predict contamination before it happens. Their FDA inspection scores are among the highest in the industry. The lesson? Proactive is cheaper than reactive. Testing after the fact is expensive. Designing it out from the start is smarter.



5 Comments
Man, I had no idea this was happening. I’ve been on generic metformin for years and never thought twice about it. Now I’m scanning every pill bottle like it’s a bomb. Thanks for laying this out so clearly - I feel like I actually understand what’s going on now.
Let’s be real - this isn’t about ‘contamination.’ It’s about corners being cut in a broken system. The FDA knew about nitrosamines for decades. They just didn’t enforce testing because generics are cheap. Now that they’re *too* cheap, they’re scrambling. Wake up, people - this is profit-driven negligence.
It’s not a crisis of chemistry - it’s a crisis of meaning. We outsource our health to corporations that treat molecules like widgets, then gasp when the widgets turn toxic. Nitrosamines are just the visible scar on an invisible wound: our surrender of biological sovereignty to the algorithmic pharmacy. We don’t need more testing. We need to stop trusting the machine.
my pharmacist just told me my new batch of losartan looks lighter. i asked if it was the ‘new formula’ and she nodded like it was no big deal. i just hope they fixed the nitro thing. i dont wanna die from a pill that costs $4.
So… we’re all just lab rats now? 😭💊 I’m crying into my $3 generic Zantac. Who do I sue? The FDA? The chemist? My pharmacist who smiles while handing me poison? I need a therapist. And a new doctor. And maybe a bunker.