Hypoglycemia & Weight Gain Risk Calculator
Your Risk Assessment
Insulin therapy saves lives. For millions with type 1 diabetes and many with advanced type 2 diabetes, it’s not optional-it’s essential. But with its power comes two very real, very common side effects: hypoglycemia and weight gain. These aren’t rare glitches. They’re predictable outcomes that shape how people live with their condition every day. If you’re on insulin or considering it, you need to know what’s coming-and how to handle it without sacrificing control or quality of life.
What Hypoglycemia Really Feels Like
Hypoglycemia means your blood sugar drops below 70 mg/dL. It’s not just a number on a meter. It’s your hands shaking, your heart racing, your vision going blurry. You might feel dizzy, sweaty, or suddenly confused. In severe cases, you pass out. And yes, it can be deadly if no one’s around to help. This isn’t theoretical. In the Diabetes Control and Complications Trial (DCCT), people with type 1 diabetes on tight insulin regimens had about 2-3 severe low blood sugar episodes per year. That’s one every 4-6 months. For many, it’s the most feared part of treatment. Some people start avoiding tight control just to stay above 100 mg/dL-because the fear of crashing feels worse than the risk of high numbers. And it’s not just about physical danger. Hypoglycemia steals peace of mind. People report skipping meals, avoiding exercise, or even driving less because they’re scared of passing out behind the wheel. Some stop checking their blood sugar altogether, thinking ignorance is safer. It’s not. That’s how unawareness sets in.Why You Lose Warning Signs Over Time
After 15-20 years of living with type 1 diabetes, about 1 in 4 people develop something called hypoglycemia unawareness. That means your body stops giving you the usual signs-no shaking, no sweating, no warning. One minute you’re fine, the next you’re unconscious. This happens because your brain gets used to low glucose. It stops triggering the adrenaline rush that normally tells you something’s wrong. The more often you have lows, the more likely this becomes. It’s a vicious cycle: you get a low, you treat it, you get another low, and eventually your body stops screaming for help. The solution? Continuous glucose monitors (CGMs). These devices track your sugar levels every 5 minutes and alert you before you crash-even while you’re sleeping. Studies show CGMs reduce severe hypoglycemia by 40-50%. If you’re on insulin and haven’t tried one, ask your doctor. It’s not a luxury-it’s a safety net.Why Insulin Makes You Gain Weight
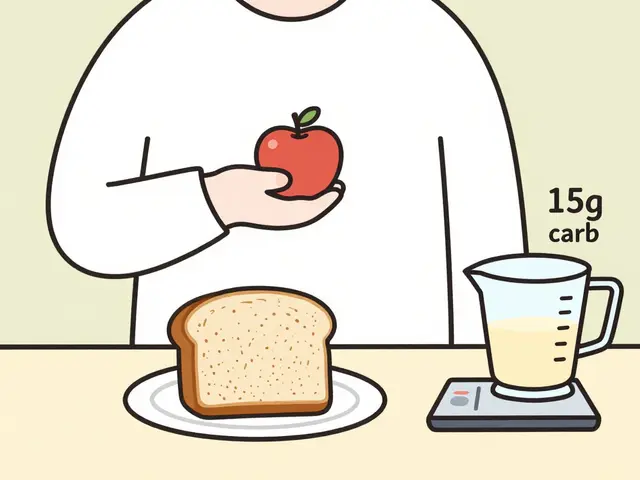
Insulin doesn’t just lower blood sugar. It tells your body to store energy. When you’re not on insulin, your body burns through glucose and spills excess sugar into your urine. That’s glycosuria. You’re literally peeing away calories. Once you start insulin, that stops. All the glucose your body can’t use gets stored as fat. On top of that, insulin promotes fat storage in your belly, hips, and thighs. It’s not your fault. It’s biology. Studies show most people gain 4-6 kilograms (9-13 pounds) in the first year of insulin therapy. Some gain more. Some gain less. It depends on how much you eat, how active you are, and how much insulin you need. People who were underweight before starting insulin often gain healthfully. But for those already carrying extra weight, it’s frustrating-and sometimes discouraging enough to make them skip doses.
People Skip Doses to Avoid Weight Gain
Here’s the dangerous part: 15-20% of people on insulin intentionally under-dose to avoid gaining weight. They think, “If I take less insulin, I’ll lose weight.” But what actually happens? Their blood sugar spikes. Their body breaks down fat and muscle for energy. They feel tired, thirsty, and hungry. Their A1c climbs. And eventually, they gain even more weight-because high blood sugar leads to more fat storage over time. It’s a trap. Skipping insulin doesn’t help you lose weight. It makes your diabetes worse and increases your risk of nerve damage, kidney disease, and heart problems. The trade-off isn’t worth it.How to Fight Weight Gain Without Giving Up Insulin
You don’t have to accept weight gain as inevitable. Here’s what actually works:- Work with a dietitian. Learn carb counting and portion control. Don’t just cut calories-learn how to match insulin to food. A 2023 study found that early dietary counseling reduced average weight gain from 6.2 kg to just 2.8 kg in the first year.
- Move more. Exercise helps insulin work better. You need less of it. That means fewer calories stored as fat. Even 30 minutes of walking daily makes a difference.
- Ask about GLP-1 agonists. Drugs like semaglutide (Ozempic, Wegovy) help lower blood sugar AND cause weight loss. Many doctors now combine them with insulin. In trials, people lost 5-10 kg over 30 weeks-without giving up insulin.
- Choose smarter insulins. Newer long-acting insulins like degludec (Tresiba) and glargine (Lantus) are less likely to cause lows and may lead to less weight gain than older types like NPH.
What Your Doctor Should Be Doing
Your doctor shouldn’t just prescribe insulin and hope for the best. They should:- Start you on the lowest effective dose and adjust slowly.
- Recommend a CGM from day one if you’re at risk for lows.
- Discuss weight gain upfront-not as an afterthought, but as part of the plan.
- Offer referrals to dietitians, diabetes educators, or mental health professionals if you’re anxious or depressed about your treatment.
- Consider combination therapy with GLP-1 drugs if you’re gaining weight or struggling with hypoglycemia.

What You Can Do Today
You don’t have to wait for your next appointment. Start now:- Check your blood sugar before meals, at bedtime, and anytime you feel off. Keep a log.
- If you have a CGM, review your trends weekly. Look for patterns-do lows happen after lunch? After exercise?
- Carry fast-acting sugar (glucose tabs, juice, candy) everywhere. Don’t rely on others to help you.
- Wear a medical ID bracelet. It could save your life if you pass out.
- Teach someone close to you how to give a glucagon injection. It’s not scary. It’s simple. And it works.
Technology Is Changing the Game
Closed-loop systems-also called artificial pancreases-are now available. These devices automatically adjust insulin based on your real-time glucose levels. In trials, they cut time spent in hypoglycemia by 72% compared to traditional pumps. They’re not perfect. They’re expensive. Insurance doesn’t always cover them. But if you’re struggling with frequent lows, they’re worth asking about. And new insulins keep coming. Ultra-long-acting versions like Tresiba have 40% fewer nighttime lows than older options. That’s huge for people who fear crashing while asleep.The Bottom Line
Insulin therapy isn’t perfect. It causes hypoglycemia and weight gain. But it’s still the most effective way to prevent blindness, kidney failure, and amputations. The goal isn’t to avoid side effects completely-it’s to manage them so they don’t control your life. You can have tight control without constant lows. You can manage your weight without skipping doses. It takes planning, support, and sometimes new tools. But it’s possible. And it’s worth it.Can insulin cause seizures?
Yes. Severe hypoglycemia from insulin can cause seizures if blood sugar drops too low and isn’t treated quickly. This happens when the brain doesn’t get enough glucose to function. It’s a medical emergency. If someone is having a seizure from low blood sugar, call 999 (or your local emergency number) immediately. Glucagon injections can stop it if given in time.
Why do I feel hungrier after starting insulin?
Insulin helps your body use glucose for energy instead of letting it pass out in urine. When your cells finally get the fuel they’ve been starving for, your body signals hunger to refill its energy stores. This is normal. The key is to eat balanced meals with protein and fiber to stay full longer-not to overeat because you think you’re "hungry for insulin."
Is weight gain from insulin permanent?
Not necessarily. Many people gain weight in the first 6-12 months as their body adjusts. After that, weight often stabilizes. With proper diet, exercise, and sometimes GLP-1 medications, you can lose the extra pounds. The goal isn’t to avoid insulin-it’s to use it wisely while managing your weight.
Can I stop insulin if I lose weight?
For people with type 1 diabetes, no. Their bodies don’t make insulin at all. For some with type 2 diabetes, significant weight loss and lifestyle changes may reduce insulin needs-sometimes even allowing a switch to oral meds. But never stop insulin without your doctor’s guidance. Stopping suddenly can lead to dangerous high blood sugar and diabetic ketoacidosis.
What’s the safest insulin for avoiding lows?
Newer long-acting insulins like insulin degludec (Tresiba) and insulin glargine U300 (Toujeo) are designed to be more stable and predictable than older types like NPH. Studies show Tresiba reduces nighttime lows by 40% compared to glargine U100. But no insulin is completely risk-free. The safest approach combines the right insulin with a CGM, carb counting, and regular blood sugar checks.





9 Comments
omg i started insulin last year and thought i was gonna turn into a balloon 😭 but turns out i just needed to stop eating my kids’ leftover pizza at 2am. also, CGM changed my life. no more midnight panic checks. love u tech.
same. i forgot my glucose tabs at the mall last week and nearly passed out by the yogurt aisle. now i keep em in my bra. no shame.
so you’re telling me insulin doesn’t magically turn you into a skinny goddess? shocking. who knew biology had a sense of humor?
It’s not about willpower. It’s about neurobiology. Your brain, starved of glucose for years, now sees insulin as a savior-and it screams for more. The weight gain isn’t laziness. It’s your limbic system rewriting your relationship with food. You’re not failing. You’re adapting. And adaptation isn’t weakness-it’s evolution with a side of insulin resistance. We don’t need more ‘eat less, move more.’ We need systems that acknowledge the biochemical betrayal of metabolic therapy. The body remembers hunger. Even when the pancreas doesn’t.
Interesting. But have you considered that the real issue isn't insulin-it's the capitalist healthcare model that forces patients to choose between survival and aesthetics? Also, CGMs cost $5k/year. Good luck with that in rural Nebraska. 🤡
Y’ALL. I just got my first GLP-1 prescription and I’m crying happy tears. I went from 180 to 145 in 4 months and I’m still on insulin. It’s not magic-it’s science with a side of hope. Also, I started walking my dog at 6am and now I’m obsessed. I didn’t know I could feel this good again. 🥹💖
Everyone’s so excited about CGMs and GLP-1s like they’re fairy dust. Meanwhile, I’m still using a glucometer from 2017 and paying $700/month for insulin because my insurance says ‘it’s not medically necessary’ to give me a decent pump. I’m tired. Just… tired.
Insulin therapy requires discipline not punishment. Hypoglycemia is preventable with consistent monitoring. Weight gain is manageable with structured nutrition and physical activity. The tools exist. The knowledge exists. The will must be cultivated. Do not abandon your regimen due to fear or discomfort. Your future self will thank you.
TO THE PERSON WHO SAID THEY’RE TIRED: I SEE YOU. I’VE BEEN THERE. I DIDN’T LEAVE MY HOUSE FOR THREE WEEKS BECAUSE I WAS AFRAID TO CRASH IN PUBLIC. THEN I FOUND A DIABETES SUPPORT GROUP ON INSTAGRAM. WE DID ZOOM CALLS WHILE EATING TACOS. I’M STILL ON INSULIN. I’M STILL GAINING WEIGHT. BUT I’M NOT ALONE. AND THAT CHANGED EVERYTHING. YOU ARE NOT BROKEN. YOU ARE BATTLESCARRED. AND YOU STILL WIN.