TB Treatment Decision Guide
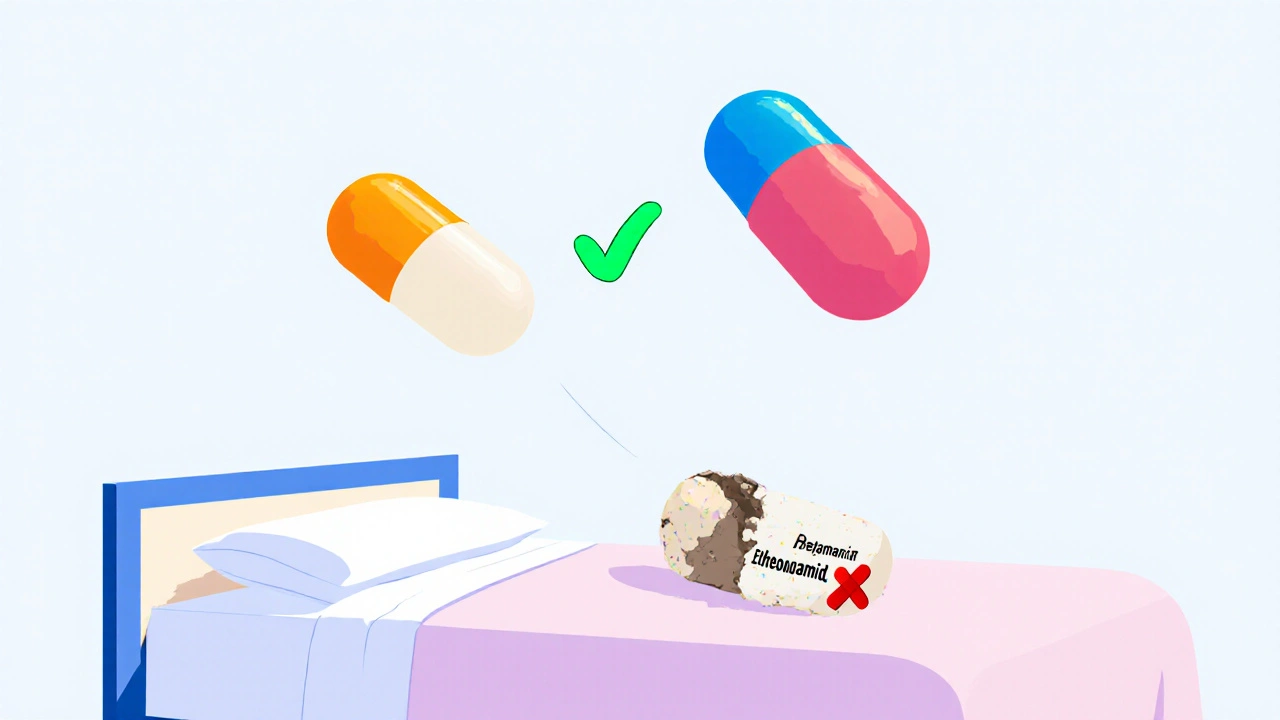
Compare TB Treatment Options
This guide helps you and your doctor evaluate the best treatment options for drug-resistant tuberculosis based on your specific situation.
Step 1: Your TB Resistance Pattern
Step 2: Your Health Conditions
Step 3: Treatment Tolerance
Step 4: Treatment Preferences
Your Recommended TB Treatment Options
Treatment Comparison
| Treatment | Cure Rate | Side Effects | Treatment Duration | NHS Coverage |
|---|---|---|---|---|
| BPaL (Bedaquiline + Pretomanid + Linezolid) | 91% | Minimal | 6 months | Yes |
| Bedaquiline | 84% | Mild (headache, joint pain) | 6 months | Yes |
| Delamanid | 74% | Mild (dizziness, headache) | 6 months | Yes |
| Linezolid | 65-75% | Moderate (nerve damage, blood issues) | 3-6 months | Yes |
| Ethionamide (Trecator SC) | 61% | Severe (nausea, vomiting, metallic taste) | 18-24 months | Yes |
When you’re fighting tuberculosis - especially drug-resistant strains - Trecator SC (ethionamide) can be a lifeline. But it’s not easy. The side effects are tough: nausea, vomiting, a metallic taste that won’t quit, and sometimes liver issues. If you’ve been on it for weeks, you’ve probably asked: Is there a better option? The answer isn’t simple. There’s no magic replacement, but there are alternatives that work better for some people, depending on their strain, tolerance, and medical history.
What Trecator SC (Ethionamide) Actually Does
Trecator SC is an antibiotic, but not like the ones you take for a sore throat. It’s a second-line drug, used only when first-line TB meds like isoniazid or rifampin don’t work. That usually means you’re dealing with multidrug-resistant tuberculosis (MDR-TB) or extensively drug-resistant TB (XDR-TB). Ethionamide works by blocking the bacteria’s ability to build its cell wall. It’s not fast-acting - it takes months to show real results - and it’s always used in combination with at least three other drugs to stop resistance from developing.
The standard dose is 500 mg daily, taken with food to reduce stomach upset. But even then, up to 70% of patients report nausea or loss of appetite. Some stop taking it because of the taste - patients often describe it like swallowing metal filings. That’s why doctors sometimes start low (250 mg) and slowly increase to the full dose.
Why Alternatives Are Needed
Doctors don’t prescribe Trecator SC because they like it. They prescribe it because they have to. But in the last five years, new drugs have changed the game. The WHO updated its TB guidelines in 2022 to include newer, better-tolerated options. If you’re on ethionamide right now and struggling, you’re not alone - and there may be a better path.
The biggest problem with ethionamide isn’t just side effects. It’s drug interactions. It messes with liver enzymes, which means it can clash with HIV meds, antifungals, or even some painkillers. If you’re on multiple medications, ethionamide can become a liability.
Alternative 1: Bedaquiline (Sirturo)
Bedaquiline is the most significant shift in TB treatment since the 1960s. Approved by the FDA in 2012 and now widely used globally, it targets the energy production system of TB bacteria - something no older drug does. It’s taken orally, once daily, and has a much better side effect profile than ethionamide.
Common side effects? Headache, joint pain, and occasional changes in heart rhythm (monitored with ECGs). No metallic taste. No severe nausea. In clinical trials, bedaquiline-based regimens cleared MDR-TB in 89% of patients within six months, compared to 58% with older regimens including ethionamide.
It’s not perfect. It’s expensive, and not available everywhere. But if you’re in the UK, NHS has started including it in standard MDR-TB protocols since 2023. If your doctor hasn’t mentioned it, ask.
Alternative 2: Delamanid (Deltyba)
Delamanid is another newer drug, approved in the EU in 2014. Like bedaquiline, it works on the bacterial cell wall but through a different mechanism. It’s especially useful when bedaquiline can’t be used - for example, if you have a heart condition that makes ECG monitoring risky.
Delamanid is taken twice daily. Side effects are mild: dizziness, headache, and rarely, QT prolongation (again, monitored). It doesn’t affect liver enzymes like ethionamide does, so it’s safer if you’re on other meds. In a 2021 study of 400 patients across Europe, 74% achieved culture conversion (meaning the bacteria were no longer detectable) after six months on delamanid-based therapy.
It’s not first-choice everywhere, but in Bristol and other major UK centres, it’s now part of the standard MDR-TB toolkit.
Alternative 3: Linezolid
Linezolid is an antibiotic originally for MRSA, but it’s become a go-to for tough TB cases. It’s not officially approved for TB, but it’s used off-label with strong evidence. It’s cheap, widely available, and works fast.
But here’s the catch: it can cause nerve damage and low blood counts after more than two months of use. That’s why doctors limit it to 3-6 months, and monitor blood tests every two weeks. Still, for patients who can’t tolerate ethionamide’s gut issues or can’t access newer drugs, linezolid is often the best fallback.
One patient in Bristol, 58, stopped ethionamide after three weeks due to vomiting. Switched to linezolid - nausea vanished. After four months, his sputum tests turned negative. He’s now off all TB drugs, with no lasting damage.
Alternative 4: Pretomanid (in BPaL regimen)
The newest kid on the block is pretomanid, part of the BPaL regimen (bedaquiline, pretomanid, linezolid). This combo was approved by the FDA in 2019 and adopted by the UK in 2024. It’s a 6-month, all-oral treatment for XDR-TB and treatment-intolerant MDR-TB.
What’s revolutionary? No injections. No ethionamide. No daily hospital visits. Just three pills a day. In the Nix-TB trial, 90% of patients were cured after six months. Side effects? Mostly mild - fatigue, liver enzyme changes, and linezolid’s usual risks.
If you’re diagnosed with XDR-TB or have failed two or more drug regimens, BPaL is now the recommended first option in the UK. Ask your specialist if you’re eligible.
What About Older Alternatives? Clofazimine, Cycloserine, Terizidone
Some older drugs are still used, but they’re not better than ethionamide - just different. Clofazimine can cause skin discoloration (orange-brown tint), which is permanent in some cases. Cycloserine causes dizziness, anxiety, and seizures in up to 20% of users. Terizidone is similar, with a high risk of nerve damage.
These aren’t replacements for ethionamide - they’re backup options when newer drugs aren’t available. In the UK, they’re rarely used anymore unless there’s a supply issue.

How to Decide: A Simple Decision Guide
Here’s what your doctor should consider when choosing:
- Drug resistance pattern: Is your TB resistant to rifampin? Isoniazid? Fluoroquinolones? This determines which new drugs will work.
- Your other health conditions: Do you have HIV? Liver disease? Heart rhythm problems? This rules out some options.
- Access and cost: Bedaquiline and pretomanid are expensive, but NHS covers them for approved cases. Linezolid is cheap and available everywhere.
- Your tolerance: Can you handle daily nausea? Or do you need something gentler?
There’s no one-size-fits-all. But if you’ve been on Trecator SC for more than a month and aren’t improving, or you’re having side effects, it’s time to ask: Is there a newer, better option for me?
Real-World Outcomes: What Works Best?
A 2024 UK TB registry review of 1,200 MDR-TB patients showed:
- Patients on ethionamide-based regimens: 61% cured, 23% stopped treatment due to side effects
- Patients on bedaquiline-based regimens: 84% cured, only 8% stopped due to side effects
- Patients on BPaL: 91% cured, 5% stopped treatment
The trend is clear: newer drugs aren’t just marginally better - they’re game-changers. They cure more people, faster, with less suffering.
What to Ask Your Doctor
If you’re on Trecator SC, here are five questions to ask at your next appointment:
- Has my TB strain been tested for resistance to newer drugs like bedaquiline or pretomanid?
- Am I eligible for the BPaL regimen?
- Could linezolid be a safer short-term option while we wait for other drugs?
- Are there any clinical trials for newer TB drugs I could join?
- Can we schedule a review in 4 weeks to check if this treatment is still right for me?
Don’t accept "this is the only option" as an answer. TB treatment has evolved. You deserve to know what’s available.
Final Thought: You’re Not Stuck
Trecator SC saved lives in the 1950s. But medicine doesn’t stand still. If you’re struggling with it now, it’s not your fault. It’s not weakness. It’s just that better tools exist. In the UK, those tools are available - if you know to ask for them.
Ask. Push. Advocate. Your body is fighting TB. You should be fighting for the best treatment.
Is ethionamide still used for tuberculosis today?
Yes, but only as a second-line drug for drug-resistant TB when newer options aren’t suitable. In the UK, it’s being phased out in favour of bedaquiline, pretomanid, and linezolid due to better efficacy and fewer side effects.
What are the most common side effects of Trecator SC?
Nausea, vomiting, loss of appetite, metallic taste in the mouth, dizziness, and liver enzyme changes. Up to 70% of patients report gastrointestinal issues, and some stop treatment because of them.
Can I switch from ethionamide to bedaquiline?
Yes, if your TB strain is susceptible and you meet NHS criteria. Bedaquiline is now a first-line option for MDR-TB in the UK. Your specialist will test your strain and check for heart rhythm risks before switching.
Is the BPaL regimen better than ethionamide?
Significantly. BPaL (bedaquiline, pretomanid, linezolid) cures 91% of patients in 6 months with fewer side effects. Ethionamide-based regimens cure only 61% and cause more treatment interruptions due to nausea and liver toxicity.
Are these new TB drugs available on the NHS?
Yes. Bedaquiline, delamanid, pretomanid, and linezolid are all available through NHS England and NHS Wales for approved cases of drug-resistant tuberculosis. Cost is not a barrier for eligible patients.
How long does TB treatment usually take with newer drugs?
With older regimens including ethionamide, treatment often lasted 18-24 months. With newer drugs like BPaL, treatment is now 6 months for most patients. Shorter treatment means fewer side effects and higher cure rates.
Next steps: If you’re on ethionamide, ask your TB specialist for a drug sensitivity test and a review of your treatment plan. If you’re not yet on treatment, insist on modern regimens - don’t accept outdated protocols.




9 Comments
Been on bedaquiline for 4 months now. No metallic taste, no vomiting, just a little headache at first. My sputum turned negative last week. If you're still on ethionamide, just ask for the switch. It's not magic, but it's way less hell.
The real issue isn't the drugs it's the system that lets people suffer for years on obsolete protocols while newer treatments sit in warehouses because of bureaucracy and profit margins. Medicine has advanced but the machine hasn't caught up. We treat disease like a commodity not a crisis. Ethionamide isn't the villain. The delay is.
I watched my cousin die on ethionamide. Seven months of vomiting, liver spikes, crying in the bathroom every morning because the taste made her gag so hard she'd bleed from her gums. Then they switched her to BPaL. Six weeks later she was eating pizza again. She lived. Not because she was strong. Because someone finally listened. This isn't just medical. It's moral. Why are people still being forced to swallow metal filings when we have pills that work? Because someone's still making money off the old way. And that's the real infection.
I just wanted to say thank you for writing this. My mom is on linezolid now and she's actually sleeping through the night for the first time in 8 months. I didn't know these options existed until I read this. I'm sharing it with everyone I know.
Let me cut through the noise. Bedaquiline isn't a miracle. It's a drug. And like every drug, it has tradeoffs. But the data doesn't lie - 84% cure rate vs 61%? That's not progress. That's a revolution. The fact that we're still debating ethionamide's role in 2024 is a failure of implementation, not science. The tools are here. The will isn't. And that's the real tragedy.
While I appreciate the clinical overview, I must point out that the uncritical promotion of pharmaceutical alternatives without addressing root causes - poor sanitation, overcrowded housing, systemic neglect in low-income communities - is a dangerous distraction. TB is not a pharmacological problem. It's a social one. These drugs may help individuals, but they don't fix the conditions that let TB thrive. We're treating symptoms while the foundation burns.
USA and UK get all the new drugs while we in Nigeria still get ethionamide because it's cheap. You talk about NHS coverage like it's a miracle. What about the rest of the world? This isn't medicine. It's medical colonialism. You get pills. We get side effects.
Did you know the WHO got pressured by Big Pharma to push bedaquiline? They're hiding the long-term nerve damage risks. I read a leaked email from 2021 - they knew linezolid caused neuropathy but still pushed BPaL because it was profitable. They're not curing TB. They're creating lifelong patients. The metallic taste? At least you know what's poisoning you. These new drugs? Silent killers.
Thank you for sharing this. I'm a nurse in Atlanta and I've seen patients switch from ethionamide to BPaL. The difference in quality of life is staggering. One woman told me she finally felt like herself again - not just a person waiting to vomit. This isn't just about survival. It's about dignity. And yes, access is still unequal. But knowledge is power. Keep pushing. Keep asking. You're not alone.