When you’re diagnosed with atrial fibrillation (AFib), the first thing you hear is that your heart is beating irregularly. But what comes next isn’t just about slowing down your heart-it’s about choosing the right path to protect your brain, your life, and your daily energy. Two main strategies exist: rate control and rhythm control. And neither works without stroke prevention. The old advice was simple: take a beta-blocker, keep your heart under 110 beats per minute, and call it a day. But that’s not the full story anymore.
What Rate Control Really Means
Rate control isn’t about fixing your heartbeat-it’s about managing the damage it causes. The goal? Keep your ventricles from racing too fast, even if your atria are still quivering. Studies like RACE II showed that letting your resting heart rate go up to 110 beats per minute is just as safe as trying to keep it below 80. That’s a game-changer. It means fewer pills, less monitoring, and less stress over hitting a perfect number.Common drugs for rate control include beta-blockers like metoprolol, calcium channel blockers like diltiazem, and sometimes digoxin. But digoxin isn’t always the best pick. In emergency rooms, amiodarone works faster and more reliably for sudden rapid AFib. Still, for long-term use, most doctors start with metoprolol because it’s cheap, well-studied, and doesn’t mess with your lungs or thyroid like amiodarone can.
Rate control is often the first move for older patients-especially those over 75-with other health problems like kidney disease, COPD, or diabetes. Why? Because antiarrhythmic drugs can cause more harm than good in frail bodies. If you’re not dizzy, short of breath, or exhausted from your AFib, rate control gives you stability without the side effects.
When Rhythm Control Makes Sense
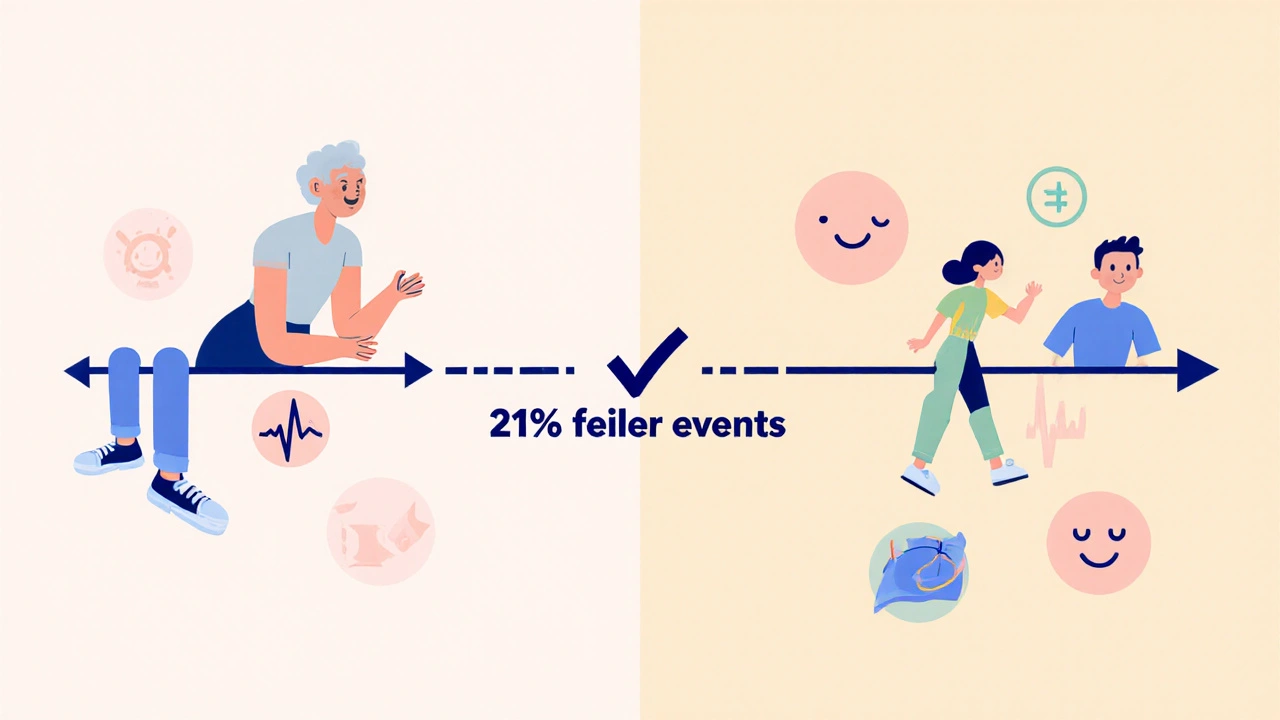
Rhythm control tries to fix the root problem: getting your heart back into normal sinus rhythm. This used to mean shocks, risky drugs, and a high chance of AFib coming back. Now? It’s different. Catheter ablation has gotten much safer. Complication rates have dropped from over 20% in the early 2000s to under 5% today. Newer drugs like dronedarone and flecainide are cleaner and more predictable than amiodarone.The big shift came with the EAST-AFNET 4 trial in 2020. It followed nearly 2,800 people with newly diagnosed AFib-most under 70-and compared early rhythm control to standard rate control. After five years, those who got rhythm control (either with drugs or ablation) had 21% fewer major events: fewer heart attacks, strokes, heart failure hospitalizations, and deaths. That’s not a small difference. It’s a 3.9% absolute reduction in risk over five years. For a 65-year-old with AFib, that’s like avoiding one major event for every 25 people treated early.
Who benefits most? Younger patients (under 65), those with paroxysmal AFib (that comes and goes), people with heart failure, and anyone still struggling with symptoms even on rate control. If you’re 58 and your AFib wakes you up at night, or you can’t walk up the stairs without gasping, rhythm control might be your best shot at getting your life back.
Stroke Prevention: The Non-Negotiable
Here’s the hard truth: whether you’re on rate control or rhythm control, you still need blood thinners. The AFFIRM trial showed that most strokes in AFib patients happened because people stopped their anticoagulants-or their INR levels were too low. Even if your heart rhythm looks normal after an ablation, your risk of stroke doesn’t vanish overnight.Doctors use the CHA₂DS₂-VASc score to decide who needs anticoagulation. A score of 2 or higher? You’re at higher risk. That means even if you’re young and active, if you’ve had high blood pressure, diabetes, or are over 75, you need a blood thinner. Direct oral anticoagulants (DOACs) like apixaban or rivaroxaban are now preferred over warfarin because they’re easier to manage and carry less bleeding risk.
Don’t assume rhythm control eliminates stroke risk. A 2023 European Society of Cardiology guideline says it clearly: anticoagulation must continue regardless of the strategy you choose. Your heart may beat normally, but if you’ve had AFib, your left atrial appendage still has a tendency to clot. That’s why you can’t stop your pills just because you feel better.

Why the Guidelines Changed
Back in 2002, the AFFIRM trial said rate control was just as good as rhythm control. That shaped practice for nearly two decades. But those trials used older drugs, older ablation tech, and mostly older patients. The average age in AFFIRM was nearly 70. What worked for them doesn’t always work for someone diagnosed at 55.Today’s guidelines, especially the 2023 ESC update, reflect real progress. We now know that early rhythm control-within the first year of diagnosis-can change the long-term course of AFib. It’s not about curing it. It’s about preventing the slow, silent damage: heart muscle weakening, kidney stress, brain clots. The goal isn’t just to feel better this week. It’s to live longer, healthier, and with fewer hospital visits over the next 10 years.
That’s why doctors in the UK and Europe are now offering ablation much earlier. In the U.S., adoption is slower, but it’s picking up. If your clinic doesn’t offer early rhythm control, ask why. Is it because you’re not a good candidate-or because they haven’t updated their protocols?
Who Should Choose What?
There’s no one-size-fits-all. But here’s a simple guide:- Choose rate control if: You’re over 75, have multiple chronic conditions, are asymptomatic, or prefer fewer medications and procedures. Lenient rate control (<110 bpm) is perfectly safe and effective.
- Choose rhythm control if: You’re under 65, have paroxysmal AFib, are symptomatic despite rate control, have heart failure, or have a CHA₂DS₂-VASc score of 2 or higher. Early ablation (within 12 months) gives you the best shot at long-term benefit.
And if you’re in the middle? Say you’re 68, have mild symptoms, and your heart rate is controlled but you’re still tired? Talk to your cardiologist about a trial of rhythm control. It’s not all-or-nothing. You can start with a drug like flecainide, and if it doesn’t work, move to ablation. You’re not locked in.
What’s Next? The Future of AFib Care
Research is moving fast. The ASSERT II trial, due to report in 2025, is looking at whether early ablation helps older patients with heart failure and preserved ejection fraction-a group that hasn’t clearly benefited from rhythm control in the past. If it does, we could see rhythm control offered to even more people.Wearable tech is also changing the game. Smartwatches now detect AFib before you even feel it. That means more people are getting diagnosed earlier-right when rhythm control has the most impact. The future isn’t just about drugs and procedures. It’s about catching AFib early, acting fast, and tailoring treatment to your age, symptoms, and risk profile.
AFib isn’t just a rhythm problem. It’s a whole-body condition. And the best treatment isn’t the one that sounds most aggressive-it’s the one that matches your life, your risks, and your goals.
Is rate control safer than rhythm control?
Rate control is generally safer for older adults and those with multiple health problems because it avoids the side effects of antiarrhythmic drugs and the risks of procedures like ablation. But for younger, symptomatic patients, rhythm control can be safer long-term by reducing the risk of stroke, heart failure, and death. Safety depends on your age, health, and how early you act.
Can I stop blood thinners if my rhythm is restored?
No. Even if you’re in normal rhythm after ablation or cardioversion, you still need anticoagulation if your CHA₂DS₂-VASc score is 2 or higher. AFib leaves behind clot-prone areas in your heart that don’t disappear just because your rhythm looks normal. Stopping blood thinners too soon is one of the leading causes of stroke in AFib patients.
Which is better: ablation or drugs for rhythm control?
For most people under 70 with paroxysmal AFib, ablation is more effective than drugs at keeping you in normal rhythm long-term. Drugs like flecainide or dronedarone help but often lose effectiveness over time. Ablation has a higher success rate, especially when done early. But it’s not for everyone-access, cost, and health status matter. Some people do well with meds; others need ablation.
Does rhythm control improve quality of life?
Yes, especially for people who feel fatigued, dizzy, or short of breath with AFib. Studies show that patients on rhythm control report better energy levels, fewer hospital visits, and improved ability to exercise. If your AFib limits your daily life, rhythm control isn’t just about survival-it’s about getting your life back.
How do I know if I’m a candidate for early rhythm control?
If you’re under 75, have been diagnosed with AFib within the past year, and have symptoms-even mild ones-you’re likely a candidate. Also, if your CHA₂DS₂-VASc score is 2 or higher, or you have heart failure, early rhythm control is now recommended. Talk to your cardiologist about your age, symptoms, and risk score. Don’t wait until you’re miserable-acting early changes outcomes.
What to Do Next
If you’ve been told you have AFib and your doctor only talked about rate control, ask: "Is early rhythm control an option for me?" Bring your CHA₂DS₂-VASc score. Ask if you’re a candidate for ablation. Don’t assume that because you’re older, you’re not eligible. Many people over 70 benefit from rhythm control if they’re otherwise healthy.Wearables like Apple Watch or Fitbit can help track your rhythm at home. If you notice irregular pulses, log them. That data helps your doctor decide when to act.
And never stop your blood thinner without talking to your doctor. Even if you feel fine, your stroke risk hasn’t gone away.



8 Comments
so i read this and im like... why are they not telling us that the pharma companies are pushing ablation because it makes more money than just giving you a pill? they dont want you to know that rate control is just as good and way cheaper. i had a friend who got ablated and now his insurance raised his rates by 400% and he still gets palpitations. this is all a scam. the docs are in on it. they get kickbacks from the cath lab. dont trust the system.
the real issue here isnt whether you choose rate or rhythm control its whether you’re being treated as a person or a data point in some clinical trial. the EAST-AFNET 4 trial is compelling but it was done on relatively healthy people under 70. what about the 82-year-old with COPD and stage 3 kidney disease who just wants to sit on the porch without feeling like his heart is trying to escape his chest? the guidelines are evolving but medicine still treats aging like a disease to be fixed not a condition to be lived with. if you’re not gasping for air and your kidneys are holding up maybe you dont need a catheter shoved up your femoral artery just to feel better. sometimes stability isnt failure its grace.
Let me be perfectly clear: The 2023 ESC Guidelines are not merely recommendations-they are evidence-based, peer-reviewed, and rigorously validated. The shift toward early rhythm control is not anecdotal; it is statistically significant, with a hazard ratio of 0.79 (95% CI: 0.67–0.93) for composite cardiovascular outcomes. Furthermore, the reduction in heart failure hospitalizations (HR: 0.71) is clinically meaningful. To dismiss this as “trendy medicine” is to ignore the fundamental principles of evidence-based practice. Moreover, DOACs have revolutionized anticoagulation management, eliminating the need for INR monitoring and reducing intracranial hemorrhage risk by 50% compared to warfarin. This is not speculation-it is clinical reality.
I just want to say how much this post meant to me. I’m 59 and was diagnosed with AFib two years ago. I was terrified. I thought I was going to die in my sleep. My doctor wanted to put me on beta-blockers and call it good. But I kept asking questions. I read everything I could. I found out about ablation. I cried when I found out I could actually get my life back. Now I’m two months post-procedure and I can walk my dog up the hill without stopping. I didn’t know I was holding my breath until I stopped. This isn’t just medicine-it’s freedom. And if you’re scared, please don’t give up. Ask for help. Ask for options. You deserve to feel alive again.
Okay but like… did anyone else notice that the article didn’t mention that amiodarone turns your skin BLUE?? I saw a guy on TikTok with AFib who took it for 6 months and he looked like a Smurf. Like literally. He had to quit. And then he started doing yoga and now he’s fine?? I think the real cure is meditation and turmeric. Also why do they keep saying ‘left atrial appendage’ like it’s a secret club? I googled it. It’s just a little pouch. Why can’t they just say ‘clot factory’?? 😅
It’s funny how people treat rhythm control like it’s some magical cure. You get ablated, your heart beats normally for six months, then bam-it’s back. And now you’ve got scar tissue where your atrium used to be, and your doctor says ‘well, we can try again.’ But you’re tired of the cath lab. You’re tired of the anxiety. You’re tired of being told you’re ‘non-compliant’ because you didn’t take your pill exactly at 8 a.m. The truth? There’s no perfect solution. There’s only trade-offs. Rate control lets you live. Rhythm control lets you hope. And stroke prevention? That’s the only thing that actually saves your life. So stop romanticizing ablation. Stop pretending you’re not just buying time. And for god’s sake, don’t stop your anticoagulant because you ‘feel better.’ You’re not cured. You’re just lucky. For now.
They’re lying about the stroke risk. The real reason you need blood thinners is because the government wants to track you. Your DOAC prescription is linked to your social security number. They’re building a database of heart patients so they can predict who’s going to die next. That’s why they’re pushing ablation too-so they can implant chips in your heart. I know a guy who had a procedure and his Fitbit started showing weird spikes. He said it was ‘syncing with the hospital server.’ That’s not syncing. That’s surveillance. Don’t trust the machines. Don’t trust the pills. Don’t trust the doctors. They’re all part of the plan.
Don’t stop your blood thinner. Just… don’t.